In a special podcast series, Mark Kreidler talks to experts and advocates about the economic and racial determinants of health in the Golden State.


California’s rural healthcare services face a viral outbreak fueled by falsehoods.


While bleak, the results of the California Health Interview Survey can help determine which residents are most in need of help.


For Kaiser member Victor Gomez, getting help meant going out of network.


Immigrant rights advocate Cynthia Buiza explains Gov. Newsom’s historic plan to help immigrants receive health care.


A new survey of 150,000 Americans finds private health care consistently ranks lower than public options.


A new California bill will make it easier to take life-saving treatment to the people who need it most.
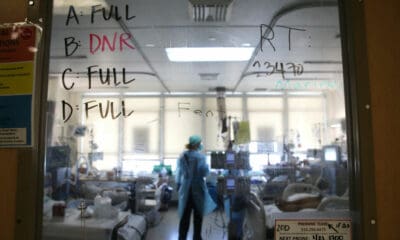

Experts describe the winter surge as a “perfect storm” driven in part by poor planning, staffing woes and a tardy governmental response.


How could only 29% of Black Californians be willing to take a vaccine that might save them?


Here are five ways the president-elect will seek to break with the policies of the past four years.

Mark Kreidler speaks with Dr. Coley King, director of homeless health care at Venice Family Clinic.


Trump claims to have cut prescription drug prices, but the proof is at the pharmacy counter.


Trump’s legal assault on Obamacare could mobilize large numbers of Latino voters against him in Florida and Texas.


The president and members of Congress are spared the search for affordable health care.


What is the president’s obligation to those sickened or killed by a virus he could have done far more to tame?


Employees call for leadership change as inspector general prepares to release first report.


Battleground states, including Florida, Arizona, North Carolina and Ohio, saw dramatic increases in the number of uninsured.


Pre-exposure prophylaxis can save lives, but patients seeking the medications face numerous obstacles.


Social and bureaucratic hurdles have caused unnecessary delays in obtaining what can be a lifesaving antiretroviral medication.


In the midst of a pandemic, some insurance companies’ profits may be even higher than had been predicted before the coronavirus hit.