Moving the Needle
Can Harm Reduction Roll Back an Epidemic of Drug-Related Deaths and Disease?
Co-published by Newsweek
The practice of harm reduction seeks not to shame people who use drugs into giving them up, but simply to provide them with the tools to improve their health.
Co-published by Newsweek
Between 1999 and 2016, deaths from opioid analgesics in the U.S. quintupled. When the pills ran out, cheap heroin flooded in.
Harm reduction for drug users, which includes everything from distributing clean needles to HIV testing to supervised injection sites, has shown to be one of the most effective strategies for slowing the spread of disease and lowering overdose rates. In some parts of California, however, the approach remains misunderstood and controversial. This week our three-part series, “Moving the Needle,” looks at the obstacles faced by harm reduction organizations in rural Northern California. Today Judith Lewis Mernit begins by reporting from the Mendocino County AIDS/Viral Hepatitis Network in Ukiah, where people who use drugs find acceptance and community without stigma or shame. Mernit’s reporting has been supported by a grant from the the University of Southern California Health Journalism Impact Fund.
Tuesday: A model harm reduction center in Humboldt County divides the city of Eureka — but also saves lives.
Wednesday: Safe injection facilities are at the front line of a health-care revolution for drug users — and of a potential showdown with the Trump administration.
Carol Chrysler is doing her best to fulfill the requests of a man sitting across from her in the cramped room of a tiny house in Ukiah, California. Chrysler, 33, is a volunteer with the Mendocino County AIDS/Viral Hepatitis Network; the man, 31, has driven 45 miles south in search of clean needles of many different gauges and lengths. “I’m a 10-pack per use guy,” he tells her, anxiously bouncing one knee. “I need 31s, 29s, 28s, 27s, half-inch, quarter inch, three-eighths.”
“I don’t have any 28s,” she informs him.
“Do you have 29s? 27s?”
“I do,” she says.
“Because I do a lot of rotation. You wouldn’t necessarily know, but I’ve been 13 years at this.”
The man, whose name I promised not to ask when he allowed me to sit in on his visit, tells me that he injects methamphetamine to endure months alone in the outback cultivating cannabis, at a grow site near the town of Laytonville. “It’s what happens when you live alone for 10 months out of the year,” he says. “I can make it about seven.” He found out about MCVHN — which locals pronounce “Macavin” — five days ago, after his last reused needle proved too dull to safely pierce his skin. He’s finding the Ukiah services a considerable step down, he adds, from the People’s Harm Reduction Alliance in Seattle, where he last lived.
“There you would show up and it was like hitting the cafeteria line,” he says. “Crack pipes, crack [pipe] condoms, cookers, everything.”
Overdose deaths skyrocketed once people figured out that dissolving and injecting newly marketed opioids for chronic pain delivered a more satisfying high than the pills did.
Chrysler politely tells him that MCVHN doesn’t do cookers. “But you’re not the first person to ask me this week,” she says, “so I’ll bring it up.”
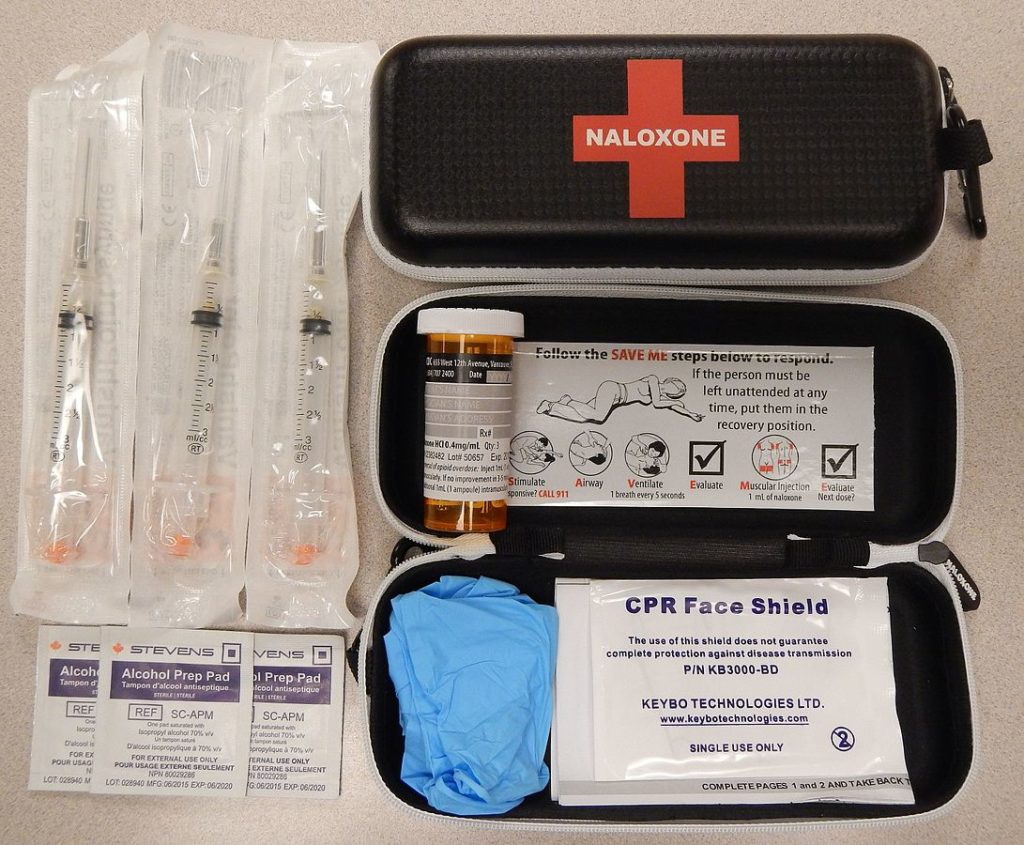
After some back and forth, Chrysler agrees to give the man two 10-packs of syringes, in two different sizes. He rejects a dose of naloxone, a drug that binds to the brain’s opioid receptors and can arrest an opioid overdose. (Meth is sometimes spiked with fentanyl, a potent synthetic opioid.) He promises that when he returns to resupply, he’ll take a test for hepatitis C, a chronic form of the disease prevalent among people who share needles.
“Next time you come in ask for Wendy,” Chrysler says. “She’ll do a test for you.”
People might find it outrageous that someone can walk in off the street and access the paraphernalia they need to inject their drugs.
Chrysler does not ask the man if he’s interested in treatment. She does not lecture him about the toll methamphetamine might be taking on his mind and body. A former methamphetamine user herself — she’s been eight months clean — Chrysler knows that if she tries that, the man might never come back. And most of all, she wants him to come back.
“Thank you, hon, see you next time,” she says as the man takes the package of supplies and hurries out. “Stay safe!”
Chrysler is a “peer leader” in the field of harm reduction, a practice that seeks not to shame people who use drugs into giving them up, but simply to provide them with the tools and support to improve their health. She started using methamphetamine as a teenager, and still understands the value of a thin, short needle when you’re injecting a second dose with shaky hands, just as she understands why it’s important to get tested for blood-borne illnesses. She is firm; she sets boundaries. But she doesn’t judge. She has been there too recently herself.
To people outside the harm reduction field, the notion that someone can walk in off the street and access, for free and without identification, the paraphernalia they need to inject their drugs might seem outrageous, maybe even criminal. “People will say, ‘You mean you give someone a new needle, and they go an inject drugs with that needle?’” said Alessandra Ross, an injection drug use specialist with the California Department of Public Health, speaking to public health professionals at a September conference on rural opioid use. “That can be a challenge for people.”
Public attitudes about offering drug users assistance without asking for sobriety haven’t changed much — even if it prevents the spread of a blood-borne disease.
But the consequences of not rising to that challenge have too recently been driven home in rural communities all over the country. Once people figured out that dissolving, cooking and injecting extended-release formulations of newly marketed opioids for chronic pain — oxycodone and oxymorphone — delivered a cheaper and more satisfying high than the pills did, overdose deaths skyrocketed: Between 1999 and 2016, the incidence of death from opioid analgesics in the U.S. quintupled. When the pills ran out, cheap heroin flooded in. And where needles were scarce, disease raged unchecked: In rural Scott County, Indiana, more than 200 people became infected with the same strain of HIV between 2011 and 2015, when then-Indiana Governor Mike Pence lifted the state’s ban on syringe-exchange services in the most affected counties. Had the state acted five years earlier, a recent Yale University study found, HIV might never have spread beyond the first 10 people who contracted it.
Harm reduction for drug users is nothing new. Even in rural America, clean-needle distribution has been going on at least since the late 1980s, when the HIV epidemic showed that it respected no urban boundaries. Libby Guthrie, MCVHN’s executive director, started out in 1987 working on HIV prevention among injection drug users in the San Francisco Bay Area, but in 1990 moved to North Carolina, where HIV was rampant throughout the 1990s and all but ignored. “I watched several people die every month in [the HIV support group I led],” she recalls, “and watched other people not talk about why they died.”
Back then, syringe-exchanges operated underground, or, in California, with emergency waivers from county officials. That wasn’t possible everywhere: Dallas Blanchard, who runs a needle exchange on Saturday afternoons in Fresno, California, remembers trying to distribute clean needles in Kern County a decade ago. “If you got caught, you’d do 10 days in jail for every syringe,” he says. But the law has progressed: Since 2012, it’s been legal to possess and distribute syringes. As of 2015, you can even buy them in a pharmacy, although in a syringe purchase trial conducted among pharmacies in Fresno and Kern counties, led by West Virginia University Professor Robin Pollini, only 21 percent of attempts succeeded.
What hasn’t changed much are public attitudes about offering drug users assistance without asking for sobriety, even if it means preventing the spread of a blood-borne disease. A recent survey conducted by researchers at Johns Hopkins Bloomberg School of Public Health found that only 39 percent of adults in the U.S. would accept a legal syringe exchange in their communities, and only 29 percent approved of safe consumption facilities, where people can inject drugs in a protected environment, in the presence of trained medical personnel.
Twenty-six counties and cities in California have some sort of syringe-exchange program, which leaves virtually the entire eastern side of the state without any such services at all. Although Blanchard says he delivers syringes over the Kern-Fresno County line once a week, and also to an outreach stop in Tulare County, neither Kern nor Tulare has a clean needle program for injection drug users, despite nontrivial rates of overdose and disease. One rural California county, Plumas, has successfully reduced its overdose-death rate — once highest in the state — with a harm reduction program that has the support of law enforcement and local officials. But in other rural counties that do have services — Fresno, Humboldt and Mendocino in particular — local opposition has remained so fierce that service providers have turned to the state for authorization, so local authorities can’t shut them down.
Money is also an issue. As the budget for health and social services in California has tightened over the past decade, harm reduction agencies have seen their resources dwindle from scarce to almost nothing. Guthrie remembers when, in the early 2000s, with funding from the state Office of AIDS, she could afford four paid, full-time outreach workers who made regular treks to the tiny northern hamlets of Laytonville and Leggett, and even Covelo, where a confederation of six Native American tribes inhabit the remote Round Valley, a one-and-a-half hour drive from Ukiah. This was important: One of the premises of harm reduction is that offering clean needles is a first point of contact with drug users who might need other health services, counseling or disease testing.
“Every day of the week,” she says, “[the outreach workers] were out doing their thing, getting fresh supplies, testing people and making referrals — ‘Do you need testing? Do you need medical care? Housing?’ They were coming face to face with people and giving them syringes once a week and coming and picking them up.”
“Their perception of an addict is that I’m a bad person. But I’m not. I have integrity. I care about other people more than I care about myself.”
Then came the Great Recession and California’s budget crisis. Facing a $40 billion budget shortfall, California in 2010 eliminated all $33 million from the Office of AIDS’s prevention budget, which had supplemented $9 million from the Centers for Disease Control. The agency was forced to spread its federal funds among 19 “high-burden” jurisdictions, most of them coastal and urban. Mendocino, Humboldt, Lake and 39 other mostly rural counties were completely left out.
“We went from riches to rags overnight,” Guthrie says. “It was like, ‘Boom! You’re done.’ I said, no, we’re not. We have people in need and we have this syringe exchange, and it’s one of the only ways to engage people who are using drugs in the county.” She has kept MCVHN running with a network of volunteers to disseminate what they can. But she admits it’s not ideal. Mendocino County covers 3,800 square miles, much of it rugged and difficult to access. “We can no longer go out and do trainings for HIV and hep C testing, we can no longer do referrals and linkages. We’ve lost that face-to-face contact with people.” Because volunteer delegates — usually people who currently use drugs themselves — collect for their friends and communities in the far reaches of the county, she says, “65 percent of our exchangers we never get to see.”
In some ways, the attention being paid to opioid dependency in the U.S. has been a boon for places like MCVHN, which had been addressing the needs of injection drug users long before substance use disorders became a national focus. When California, in June of 2018, issued a statewide standing order for naloxone, allowing community organizations to obtain and distribute the overdose-reversal drug without a physician’s guidance, the county health department turned to Guthrie for help. “We were the only agency in the county that had any experience with it,” she says.The response to the opioid crisis “means I don’t have to invite myself to the Opioid Safety Committee meetings anymore,” Guthrie says. “We’re no longer those people down the street enabling drug addicts.” With the help of a new county public health director, Barbara Howe, Guthrie is in the process of securing funding for two outreach workers for the first time in 13 years. A new police chief, Justin Wyatt, has even stepped up to serve on the county’s Homeless Action Services Group, which among other things addresses drug misuse issues among people who live without shelter.
“I’ve been six days clean and I’ve already made up my mind I’m going to go out and get loaded today. I’m dopesick.”
But “we’re still the red-headed stepchild,” says Guthrie. “Not everyone embraces what we do.” Not everyone understands, in other words, that an overdose prevention kit and revised prescribing protocols aren’t the answer to everyone’s struggle with substance use.
At MCVHN, I meet Sean Jardstrom, who’s been using methamphetamine for 34 years — since he was 14 — and injecting for 15 of them. As dogs large and small — a poodle named Snickers, a border collie, Finn — circle in and out of the room, he tells me that he’s just left his fourth attempt at rehab. “I’ve been six days clean,” he told me, “and I’ve already made up my mind I’m going to go out and get loaded today. I’m dopesick.”
Jardstrom, who is gruff-voiced and tall, dressed in cargo pants and a Yosemite National Park T-shirt, doesn’t necessarily need free needles from MCVHN. Though he’s homeless, he has enough money from his disability payments to buy them at Walgreens. He’s managed to remain both HIV- and hep C-negative, and knows enough now to stay that way. What he comes to MCVHN to find, he says, is a community of people who accept him for what he is — people he considers his adopted family, people who don’t judge him.
“I’m scared that I’m going to die an addict,” he says. “But I can’t see how I won’t.” His family — mom, stepdad, a brother and a sister —refuse to speak to him until he gets clean. “Their perception of an addict is that I’m a bad person. But I’m not. I have integrity. I care about other people more than I care about myself.”
Jardstrom and I talk for a long time, until he gets restless and has to do something else. At one point, talking about his father, the only member of his family who stood by Jardstrom until he died in 2008, he starts to cry. “He never gave up on me,” he says. “He was the only one.” I want to help him. I know I can’t. I am grateful he has found his way here.
Judith Lewis Mernit’s reporting on harm reduction in rural California was supported by the USC Annenberg Center for Health Journalism’s 2018 Impact Fund.
Copyright Capital & Main

-

 Column - State of InequalityFebruary 5, 2026
Column - State of InequalityFebruary 5, 2026Lawsuits Push Back on Trump’s Attack on Child Care
-

 Column - California UncoveredFebruary 6, 2026
Column - California UncoveredFebruary 6, 2026What It’s Like On the Front Line as Health Care Cuts Start to Hit
-

 The SlickFebruary 10, 2026
The SlickFebruary 10, 2026New Mexico Again Debates Greenhouse Gas Reductions as Snow Melts
-

 Latest NewsFebruary 12, 2026
Latest NewsFebruary 12, 2026Trump Administration ‘Wanted to Use Us as a Trophy,’ Says School Board Member Arrested Over Church Protest
-

 Latest NewsFebruary 10, 2026
Latest NewsFebruary 10, 2026Louisiana Bets Big on ‘Blue Ammonia.’ Communities Along Cancer Alley Brace for the Cost.
-

 Column - State of InequalityFebruary 12, 2026
Column - State of InequalityFebruary 12, 2026They’re Organizing to Stop the Next Assault on Immigrant Families
-

 The SlickFebruary 16, 2026
The SlickFebruary 16, 2026Pennsylvania Spent Big on a ‘Petrochemical Renaissance.’ It Never Arrived.
-

 The SlickFebruary 17, 2026
The SlickFebruary 17, 2026More Lost ‘Horizons’: How New Mexico’s Climate Plan Flamed Out Again


