“Our staffing in the ER is beyond dire now,” said Heather Fallon, a nurse in the emergency department at the Captain James A. Lovell Federal Health Care Center in North Chicago who had long been dreading the arrival of Sept. 30, the day the fiscal year came to an end.
That was the day she says she lost two nurses — and the facility lost nine staffers in total — whose contracts ended, putting further strain on her team, which has seen an increase in patients this year. Veteran Affairs Secretary Doug Collins had vowed to have reduced the size of the agency by 30,000 positions by that date without impacting health services for veterans.
“We are understaffed,” Fallon said. “We don’t have all of the services that we would have had on a regular basis.”
Meanwhile, wait times have increased for patients, said Florence Uzuegbunam, a nurse practitioner who works in primary care at a VA hospital outside of Atlanta. She also said that the staffing shortage has increased since Sept. 30 and that an increase in patients has reduced the time available for outpatients from the recommended one-hour visit to 30 minutes. “You can’t do much in 30 minutes.”
She added that in many areas of the hospital — including the women’s wellness clinic — there is reduced staffing.“I am assigned the duties of two people. Many of my co-workers told me they are putting an average of four hours unpaid daily just to keep up with the workload.”
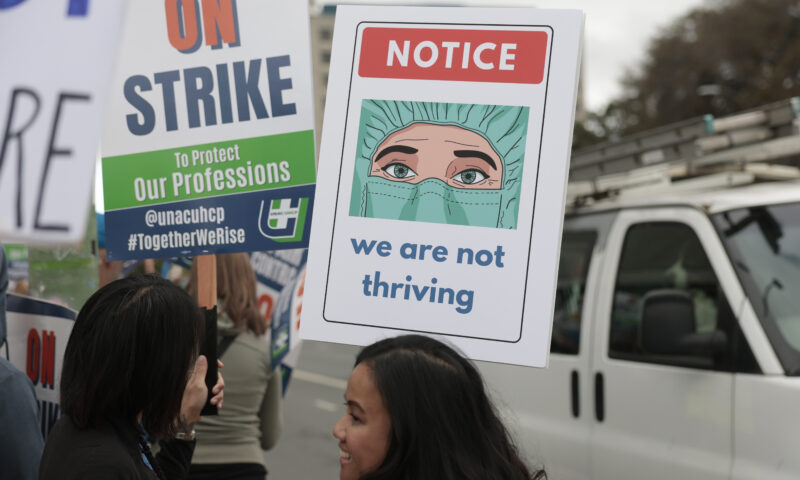
Both Fallon and Uzuegbunam are speaking out as members of National Nurses United, the largest union of registered nurses in the country, whose contract with the VA was terminated in early August. (Disclosure: NNU is a financial supporter of Capital & Main.)
The attrition of the VA workforce in the last nine months has put a strain on understaffed hospitals and clinics, hurt morale and sped up the transition to private care, nurses and veterans advocates told Capital & Main.
Collins’ decision in June to scrap a plan for massive layoffs and his promise to provide quicker services to veterans brought a sigh of relief to many and generated positive headlines.
But the upheaval caused by the Trump administration’s earlier firings of probationary employees who were then rehired months later, the closing of some VA facilities and the cancellation of medical research trials have had a major impact, say nurses who work at VA facilities, staffers at the department and veterans advocates. Morale is low, say nurses and staffers at VA facilities, who asked not to be identified out of fear of retaliation, noting that this year the VA decided not to conduct its annual staff satisfaction survey — which has been conducted every year since 2006 — citing costs. The VA confirmed that the survey was not conducted this year.
Collins has repeatedly vowed that cutting 30,000 positions won’t directly impact health care or benefits for veterans provided by the Veterans Health Administration, the healthcare branch of the VA. The VHA, which is the country’s largest integrated healthcare system, serves 9.1 million enrolled vets each year, providing care at 1,380 health care facilities.
Yet, between December 2024 and August 2025, the VA reported a net loss of thousands of health care positions — including 875 physicians, 2,403 registered nurses, 511 licensed practical nurses, 335 nurse assistants, 649 social workers, 287 psychologists and 906 medical support assistants, according to the department’s workforce dashboards, first highlighted by The American Prospect. The total number of those in mission-critical occupations — which “reflect the primary mission of the organization without which mission-critical work cannot be completed” — dropped by 4,214. For comparison, during the Biden administration, the number of those in mission-critical occupations increased from December 2023 to August 2024 by 2,806.
While the total number of U.S. veterans has been steadily declining in recent decades, the population of aging veterans is growing, with more than one-quarter of veterans now 75 and over, facing greater health risks. About 1.3 million veterans are 85 and older, a population that is expected to increase to 1.7 million in 2034.
The staffing reductions and policy changes at the VA have prompted hundreds of current and former VA doctors, nurses and other caregivers to write a letter to Collins, warning about the negative impacts. “We write to raise urgent concerns about proposed policies which, in addition to ones already enacted, will undermine VA’s healthcare system, overwhelm VA’s budget, and negatively affect the lives of all veterans.”
Peter Kasperowicz, a spokesperson for the agency, vigorously pushed back on the claims, stating that “the only staff reductions at VA have been voluntary through resignations and retirements, and these departures had no impact on VA health care, benefits or services.”
He also noted that the nurses who left the Lovell facility in North Chicago were “temporarily hired under a contract to assist with deployment of the electronic health care system at Lovell” and that they were no longer needed, adding that the facility’s nursing staff has grown since last year. Kasperowicz also said that “the Atlanta VA Health Care System has not implemented any system-wide reduction of routine outpatient visit lengths.” He added that though the facility’s women’s wellness center has one less Patient Aligned Care Team than it did last year, it is “actively hiring to fill out” an additional team.
“Struggling to Keep Up With Patient Load”
Understaffing is a persistent complaint among veterans. U.S. Army veteran Jose Vasquez, who is the executive director of Common Defense, an advocacy group for veterans, was recently diagnosed with pancreatic cancer. He credits New York’s Manhattan VA (now the Margaret Cochran Corbin VA Campus) with saving his life.
“I mean, full stop, they figured out what was going on with me, got me quickly through the diagnostic processes and got me referred to surgical oncology.”
But he said that when he was an inpatient, before and after surgery, “It was clear to me that the nursing staff was struggling to keep up with the patient load.”
Vasquez said that he has heard from other veterans with cancer who are receiving chemotherapy through the VA that “some appointments have been either delayed or cancelled.” Cancer treatment delays have been an ongoing issue at the agency for decades. The VA said it could not comment on such anonymous anecdotes without having specific details on the cases.
CNN recently reported that some VA hospitals had increased their enforcement of a policy that limits the number of long-term therapy sessions available to veterans and to “broadly reduce the number of patients who get this long-term care — without consideration for whether this is clinically appropriate,” according to mental health providers and VA patients. Kasperowicz, a spokesperson for the agency, told CNN that there are no limits on the number of VA appointments that patients can have in mental health and other areas.
In September, veterans with amyotrophic lateral sclerosis, known as Lou Gehrig’s disease, testified before the Senate Veterans’ Affairs Committee about delays they said they’ve experienced in getting medical care and supplies, as well as extended wait times for services at VA clinics and hospitals.
“For a person with my condition, this is not just an inconvenience — it’s a grave threat,” Navy veteran Shelly Hoover — who was diagnosed with the disease in 2013 — told the committee. The testimony prompted Sen. Richard Blumenthal (D-Conn.) to request an independent audit by the Government Accountability Office of the VA’s spinal cord injuries and disorders program.
In addition, the VA’s hiring freeze of medical research staffers has slowed access to clinical trials, including those aimed at preventing dementia and heart disease and studying advanced cancers, according to Sen. Patty Murray (D-Wash.), senior member of the Senate Committee on Veterans’ Affairs. She and other senators sent a letter to Collins on July 22, demanding the rehiring of “wrongly terminated researchers” and the restoration of grants revoked from VA researchers. Her staff said that Collins has not responded to her letter.
In the last several months, several researchers told Capital & Main that they have been rehired by the VA and are continuing their studies. They declined to speak on the record about their experiences, citing fears that they would face retribution.
Kasperowicz, the VA spokesperson, told Capital & Main that its department-wide vacancy rates for doctors and nurses are 13.7% and 10%, respectively — lower than the vacancy rates during the Biden administration. But veteran advocacy groups said they don’t trust those numbers because the VA is cutting positions, resulting in an artificially low vacancy rate. “If you take the position off the organizational chart as a [full-time employee], it looks like you don’t have a vacancy,” said Suzanne Gordon, the co-founder of the Veterans Healthcare Policy Institute.
The decline in the VA’s workforce leaves it incapable of handling the increase in aging vets, veterans health advocates said. “The fact is that the veteran population is older and sicker and poorer,” Gordon said. “So even if the population demand declines a small bit, the need doesn’t decline because you have these people now who are older — in addition to their military-related service conditions, they now have health conditions connected to aging.”
Jan Ruhman, a Marine Corps veteran who did two tours in Vietnam, is 78 and has had his share of medical procedures — eye surgery, Mohs surgery for skin cancer and a triple bypass operation in 2015 after a heart attack that year. He lives in San Diego and goes to the La Jolla VA, where he’s experienced “longer waiting times and people are a little more rushed.”
He said that the VA has come a long way from 1970 — he distinctly remembers the filthy conditions of the Long Beach VA hospital; he recently visited a friend there and, he said, it now has “first-class facilities.”
But he’s worried about the impact of staff cutbacks — “Every single person at that VA health care system is a critical worker” — and said, “My fear is that they’re going to take a system that became world class from being one of the worst in the world and they’re going to take it apart, piece by piece.”
During a recent visit to the Fayetteville VA Medical Center in North Carolina, Secretary Collins toured an expanded emergency department and dental clinic and told reporters: “For those who came to this area and said we’re cutting and slashing … We’re actually putting the money where it needs to be.” He added: “We’re also making sure we’re organized in such a way that we’re spending the money in a proper and efficient way.”
That includes opening new clinics and closing others, sometimes forcing veterans to travel far from their homes to get medical services. The residential substance abuse center at New York’s Brooklyn VA Medical Center “paused” admissions on May 30 due to “loss of critical staff needed to maintain a safe and effective program,” per a memo sent to staffers.
In some cases, that has forced some veterans seeking substance use treatment to be admitted to psychiatric facilities to get care, said a staffer at the Brooklyn center who asked not to be identified out of fear of retaliation. “Now when you’re trying to rehab from drugs, you don’t really need the person next to you eating his toenails,” said the staffer. “It’s not conducive to the rehab process. It’s an awful situation.”
The Brooklyn center recently reopened though it had trouble filling top slots, said Ketsia Glemaud, a mental health care nurse speaking as a member of National Nurses United who worked at the facility until May when it was shut down.
Glemaud said the situation is dire in New York City, claiming that there are not enough substance abuse clinics to meet the needs of veterans due to closures in the wake of the pandemic and budget cuts over the last eight years. She says that those who showed up at the doors of the Brooklyn facility in recent months were turned away and told to go to VA facilities in New Jersey and Westchester County, at least an hour’s drive from New York City.
“The closure of these programs has been heartbreaking for the veterans,” Glemaud said. “That’s a really difficult thing to experience, especially if you’re a veteran who’s been through hell and back and now you’re dealing with health issues or addiction. You feel abandoned.”
The VA’s Kasperowicz said that health care wait times and benefits backlogs “were worse under President Joe Biden and are getting better under President Donald Trump.” He added that the VA has opened 16 new health care clinics since January and that the backlog of veterans waiting for VA benefits increased 24% under Biden and is down more than 37% during the second Trump administration.
In addition, Kasperowicz said the backlog of veterans waiting for VA benefits is down 49% since Jan. 20, 2025, after it increased 24% during the Biden Administration; that the agency is processing record numbers of disability claims, “reaching an all-time fiscal-year high of three million claims”; that it has offered veterans more than 1.4 million appointments outside of normal operating hours since Trump took office; and that it is spending an additional $800 million on infrastructure improvements “to ensure department facilities provide safe and effective patient care.”
Pushing Patients Into the Private Sector
Ruhman, the Marine Corp veteran, said he’s also concerned about the VA’s move to push more veterans into private care through a program called Community Care, which allows vets to get reimbursed for care at non-VA medical facilities. He said that his experience with the program did not give him confidence — claiming he had to wait five weeks to get a referral for rehab services after his triple bypass surgery. “You wait too long — and they’re not prepared to deal with veterans — and that has been the experience of many people.”
The rationale for the program is universally supported — especially for vets who require specialized care or live far from VA clinics — but it has been criticized for lack of oversight, its increasing cost and concerns that it potentially weakens the VA’s own services.
Mandatory spending for Community Care is projected to increase from $6.74 billion in fiscal year 2024 to $9.77 billion in fiscal year 2025, though “the evidence does not bear out Community Care as a meaningful replacement for VA direct care,” said Dr. Kyleanne Hunter, a former Marine Corps combat helicopter pilot who now runs Iraq and Afghanistan Veterans of America (IAVA). In testimony before the House Veterans Affairs Subcommittee on Health last month, she noted that only 31% of IAVA members felt that Community Care providers understood their medical needs and stated that direct care received at the VA has “markedly better patient outcomes” when compared to Community Care at non-VA facilities.
“The VA system was built with the veteran as its heart. Private sector medical care has been built on a system of profit maximization. These two systems may be at odds when it comes to veteran outcomes; their philosophies and models of care are that different,” Hunter said. “This is born out in the evidence. Recent studies found that Community Care providers frequently administered high-cost and medically unnecessary procedures to veterans in order to maximize the money received from the government.”
In addition, a recent study funded by the VA of 62,911 veterans with mental health conditions showed “significantly lower ratings of experiences” with Community Care when it came to overall satisfaction, clinician rating, waiting times and billing.
Veterans say that Community Care can be an important component of health services, but it needs to be improved and not weaken the VA. “If you don’t fund the VA direct care system, Community Care could cause it to collapse and we are very close to that,” said Ruhman.
Kasperowicz said that the second Trump administration “has already made a number of improvements to Community Care capabilities,” including extending the length of new VA Community Care authorizations to one year for 30 standardized types of care and removing secondary approval requirements for veterans to access non-VA care.
That second provision has been criticized by veterans advocates, who claim that it removes an important oversight function. “That’s the reason why the private sector loves the VA and the Community Care program, because there’s no effective utilization review,” said Gordon, the co-founder of the Veterans Healthcare Policy Institute. “That’s unheard of in the private insurance market or even Medicare.”
Copyright 2025 Capital & Main

 Column - State of InequalityJanuary 22, 2026
Column - State of InequalityJanuary 22, 2026
 The SlickJanuary 20, 2026
The SlickJanuary 20, 2026
 Latest NewsJanuary 21, 2026
Latest NewsJanuary 21, 2026
 The SlickJanuary 19, 2026
The SlickJanuary 19, 2026
 Latest NewsJanuary 22, 2026
Latest NewsJanuary 22, 2026
 The SlickJanuary 23, 2026
The SlickJanuary 23, 2026
 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026
 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026

