Calm, soft-spoken nurse Gabriella Oloye considers her words carefully when she tells me about one of her recent home visits with an immigrant patient.
When the 6-foot-8-inch tall Oloye walked into a South Los Angeles apartment for an appointment with a middle-aged mother in June, the nurse noticed luggage near the door. The woman, an undocumented immigrant, had decided to self-deport and move her family back to Mexico.
Her children worried that she and her husband had jeopardized their safety by attending their child’s middle school graduation earlier in June. While their children are U.S. citizens and want to stay in Los Angeles, the parents feel it is safest to return to Mexico.
“It feels like what I read in middle school about World War II with people hiding, not going out, not going to parks,” Oloye says. “You can see [fear] in their eyes.”
“Or in the tone of their voice,” adds her colleague Peggy Hernandez, a medical assistant.
Oloye, Hernandez and Isaac Palacios make up one of two mobile medical teams for St. John’s Community Health in South Los Angeles whose mission is to navigate around the atmosphere of fear in immigrant communities, where those without legal status have become reluctant to leave home, even for medical reasons.
The three-person team’s visits are part of the Health Care Without Fear program the community health organization launched earlier this year to bring health care directly to the homes of undocumented patients afraid to visit one of its clinics.
While the trio does its best to care for unattended health needs — unmonitored blood pressure, diabetes and infections — the team is also witness to the on-the-ground impacts of the Trump administration’s blunt-force immigration policy of at-large arrests and deportations and how it is harming public health by prompting some patients concerned about their immigration status to avoid medical care.
Two teams are mobilized daily. Each drives in a cramped Ford Transit Connect van compact enough for the small team and their supplies to fit into tight parking spaces in urban neighborhoods. I don’t know how 6’8” Oloye makes it work.
* * *
St. John’s Community Health is a network of 24 clinics and four mobile units across Central and South Los Angeles as well as Compton. St. John’s treats more than 120,000 low-income patients who receive Med-Cal or are uninsured or underinsured.
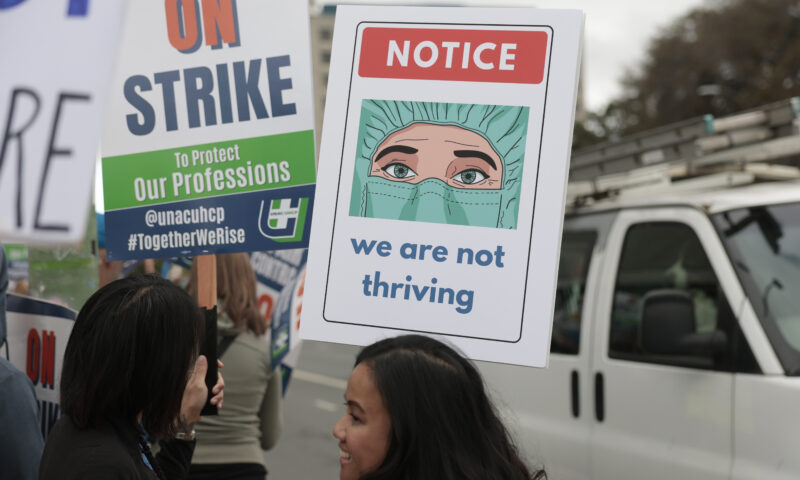
Health Care Without Fear was announced in March, and the project has ramped up its work since June. That’s when the Trump administration began targeting California with an aggressive wave of immigration enforcement operations using heavily armed and masked federal agents.
The raids have largely netted people without violent criminal convictions, according to the Cato Institute, a libertarian think tank. American citizens have also been detained by immigration agents.
I meet the mobile team in late June in the parking lot of what staff call St. John’s HQ in South L.A. after they spent the morning driving to patient homes south of downtown Los Angeles. The trio is visibly exhausted, walking slow and speaking softly, their shoulders slightly slumped as we talk.
How do medical professionals maintain preventive health care for scared patients in this environment, I ask.
“We’re learning as we go,” responds Hernandez.

Isaac Palacios, a driver with St. John’s Community Health, transports mobile medical teams to the homes of undocumented patients.
The day starts around 8:30 a.m., when the team arrives to review files for the day. They pack based on the needs of the patients they will see. They take vials and syringes for blood tests, cups for urine and stool samples, prescription refills as well as equipment to check blood pressure and heart rate.
The team also has to consider the route they will be taking. If blood or other samples need to go back to a lab, the team returns to St. John’s HQ. If not, they will break for lunch wherever they are before attending to the next patient.
They take great care to make sure there are no surprises. Hernandez calls patients in advance to confirm the appointment and then again when they arrive.
“They feel they can trust no one,” Hernandez explains. “Not even to open the door.”
The team gives themselves 45 minutes to travel to each patient. Considering traffic, even with streets visibility less congested during the summer school break, 45 minutes from door to door across South Los Angeles is not that much time.
Palacios, the team’s driver, considers safety issues, like parking, traffic flow and whether there have been reported immigration raids nearby. An immigrant himself, Palacios carries his paperwork authorizing him to live and work in this country. Still, he worries he could be swept up by federal agents like other immigrants, even with documentation.
“Sí, pero still; they don’t care,” Palacios says.
Oloye says she has become more cautious with her phone, afraid immigration might try to track metadata from social media.
Once the team enters a patient’s home, they begin a typical clinic visit: checking blood pressure, heart rate, following up on known chronic conditions and asking about new health concerns. In the past three weeks, Oloye says, they have seen patients who risked going without care for uncontrolled diabetes, nerve damage, high blood pressure, pneumonia and other infections.
The Health Care Without Fear program was created after clinic staff noticed an increase in missed appointments in the first two months of this year and realized there was a potential public health emergency. Jim Mangia, the president and CEO of St. John’s, told Capital & Main in June that the percentage of patients who were not showing up for their scheduled appointments had spiked to 25%-30% — nearly triple the typical number. Patients were not coming in because they were afraid of the increasingly brazen ICE raids around Los Angeles early in President Trump’s second term.
* * *
Donald Trump has targeted Mexican immigrants since he first came down that gold-colored escalator and announced his presidential ambitions in 2015. What began with a pair of coordinated raids on June 6 in Los Angeles’ Fashion District and a nearby Home Depot escalated into a widespread assault on the region’s Latino community.
Social media and local news in Los Angeles are awash with recordings of masked men brandishing rifles, gas and flash bang grenades and refusing to identify themselves as they grab people off the street. In response, residents have formed community-defense groups to protect those targeted for arrest and deportation.
A July 11 temporary restraining order against the Trump administration’s mass deportation tactics that was upheld earlier this month by the 9th U.S. Circuit Court of Appeals has slowed, though not ended, ongoing raids. U.S. and Customs and Border Protection have made more than 4,000 arrests in the Los Angeles area since June 6, though the number of arrests dropped significantly in July, the Los Angeles Times reported.

St. John’s Community Health has seen an increase in undocumented patients avoiding medical appointments. This waiting area in the clinic parking structure is usually occupied, but was empty on July 3.
* * *
Before I meet the mobile team, a St. John’s staffer introduces me to a patient, an undocumented woman from Mexico whose identity we agree I would not reveal. She reluctantly came in for doctor’s appointment that day after Ana Ruth Varela, a community health support organizer, or promotora, with St. John’s, agreed to walk the woman from her home nearby, accompany her to the clinic for her appointment and return her home. The woman’s young adult sons called multiple times to check on their mother’s whereabouts and safety.
The woman has been going to St. John’s for years, since her children were born.
As we speak in Spanish, I notice that she’s suddenly shaking, with twitches and spasms in her arms, neck and head. I would try to find comforting words to calm her; she smiled when I say that I play son jarocho, the traditional music of her region in Mexico. But her involuntary movements interrupt her speech. She says she is shaking because she is scared and anxious about the raids and abductions.
She was there for a regular checkup and to get her blood pressure taken. She noted it was high but played it down and insisted she was OK. A staff member warned the woman, however, that in fact her blood pressure was very high and worrisome.
Concerned with her symptoms, I try to end our interview, but she continues speaking.
The masked men with rifles and no identification rampant across Los Angeles reminds the woman of the narcos, drug-trafficking cartels, that invaded her rural home along Mexico’s Gulf Coast as a child, she tells me. When the narcos would come, she and the other children would flee and hide among the nearby trees and bushes. Their signal to return was their mother singing.
Many patients are sharing similar memories of the places they fled as they see masked men in the streets of Los Angeles, Varela says; the raids are triggering post-traumatic stress disorder.
While the mobile teams are deployed to tend to patients’ physical wellbeing, Oloye has since June begun asking them about their mental health during checkups. Oloye asks how they are feeling, probing for signs of depression, anxiety and stress. She has seen patients who need medication for depression and anxiety.
In her calm and steadfast voice, Oloye notes that adding a psychiatrist or psychologist to the team would be helpful. She says patients who have been staying home from work also need rent support and money for food and to pay bills.
Oloye sighs as she considers the gravity of what she has witnessed.
“I wish I could do more,” she says.
Copyright 2025 Capital & Main.
Photos by Barbara Davidson.

 Column - State of InequalityJanuary 22, 2026
Column - State of InequalityJanuary 22, 2026
 The SlickJanuary 20, 2026
The SlickJanuary 20, 2026
 Latest NewsJanuary 21, 2026
Latest NewsJanuary 21, 2026
 The SlickJanuary 19, 2026
The SlickJanuary 19, 2026
 Latest NewsJanuary 22, 2026
Latest NewsJanuary 22, 2026
 The SlickJanuary 23, 2026
The SlickJanuary 23, 2026
 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026
 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026



