Society
Scenes from L.A.'s 'Fight for $15'
About one thousand Angelenos marched and rallied for a $15 minimum wage near downtown Los Angeles Wednesday. While several protests occurred at fast-food outlets and other locations across the city early in the morning, the main event began shortly before lunchtime, when demonstrators gathered at a McDonald’s located on Figueroa and 28th streets, and then marched to the Tommy Trojan statue on the University of Southern California campus.
Part of a nationwide Tax Day protest, L.A.’s Fight for $15 marchers included Walmart workers, members of California’s In-Home Health Supportive Services and part-time instructors from USC. One university activist named Maria told Capital & Main that she was a first-generation college student from a working class family. She claimed that USC is pitting the needs of students against raising the incomes and working conditions of part-time academic employees.
“Some faculty are not making ends meet — they’re similar to airport workers,” she said. “Hiring part-time workers is the equivalent of using sweatshop labor.”

-
 Column - State of InequalityJanuary 22, 2026
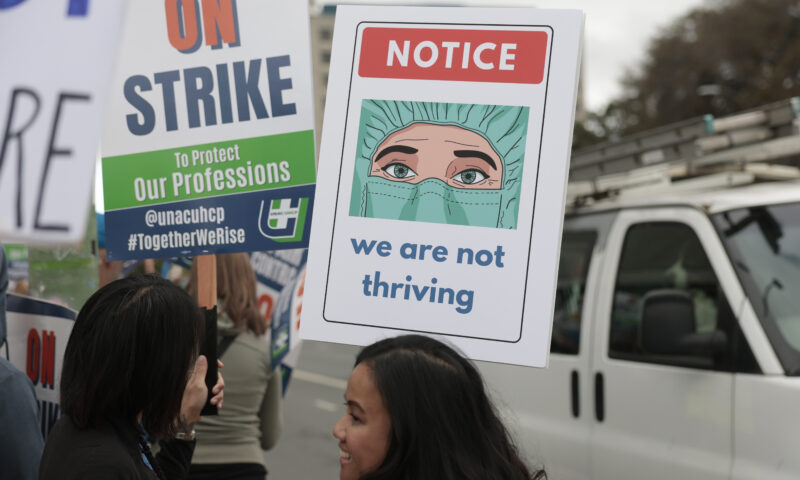
Column - State of InequalityJanuary 22, 2026On Eve of Strike, Kaiser Nurses Sound Alarm on Patient Care
-

 The SlickJanuary 20, 2026
The SlickJanuary 20, 2026The Rio Grande Was Once an Inviting River. It’s Now a Militarized Border.
-

 Latest NewsJanuary 21, 2026
Latest NewsJanuary 21, 2026Honduran Grandfather Who Died in ICE Custody Told Family He’d Felt Ill For Weeks
-

 Latest NewsJanuary 22, 2026
Latest NewsJanuary 22, 2026‘A Fraudulent Scheme’: New Mexico Sues Texas Oil Companies for Walking Away From Their Leaking Wells
-

 The SlickJanuary 23, 2026
The SlickJanuary 23, 2026Yes, the Energy Transition Is Coming. But ‘Probably Not’ in Our Lifetime.
-

 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026The One Big Beautiful Prediction: The Energy Transition Is Still Alive
-

 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026Are California’s Billionaires Crying Wolf?
-

 Latest NewsFebruary 3, 2026
Latest NewsFebruary 3, 2026Amid the Violent Minnesota Raids, ICE Arrests Over 100 Refugees, Ships Many to Texas

