Pandemic Nation
Rural Clinics and Hospitals Bear the Brunt of COVID Misinformation
California’s rural healthcare services face a viral outbreak fueled by falsehoods.

The trendline in California is undeniable: Rural areas with vaccination rates well below the state average are bearing the brunt of COVID-19’s delta strain. In those regions, death rates are vastly outpacing those in urban settings. Nationally, rural areas are currently experiencing twice the death rate of urban areas.
While the first wave of the pandemic in early 2020 mostly missed the more lightly populated areas of the country, the dark script has flipped in the fall of 2021. At a time when rates of vaccination increasingly determine COVID-related outcomes, only 46% of rural residents were fully vaccinated as of mid-August. That compared with 60% of urban residents, according to researchers at Syracuse University.
The explanations are numerous. Syracuse’s team concluded that affinity for former President Donald Trump and “lower educational attainment” were the most predictive drivers of lower vaccination rates in rural areas. (Trump said earlier this month that he received the Pfizer vaccine before leaving office.) The broad spread of misinformation about the safety of the vaccines is often cited as a deterrent to efforts to inoculate rural residents, as is a false sense of security dating to early in the pandemic, when the virus was mostly infecting people in denser urban settings.
Many community health centers have been fighting to keep the doors open since early in the pandemic, when patients canceling routine preventive care caused massive drops in revenue.
But it’s important not to lose sight of the bigger picture. The reality is that rural health care in the U.S. has been under siege for years, and as the quantity and reach of that care disintegrates, so do the lines of defense against something as aggressive and unyielding as a massive viral outbreak.
The Sheps Center for Health Services Research at the University of North Carolina has tracked 181 rural hospital closures since 2005. Meanwhile, many community health centers, of which 42% are rural, have been fighting to keep the doors open since early in the pandemic, when patients staying away from doctors and canceling routine preventive care caused massive drops in revenue.
That is a brutal combination that leaves rural residents, including California’s vast agriculture economy workforce, struggling to obtain both care and access to accurate information about the COVID vaccines. Among the millions of Californians who used one of the state’s Federally Qualified Health Centers in 2019, 18% were uninsured or paid out of pocket and another 64% relied on Medi-Cal. All are in need of quality care.
* * *
Financial crises among community clinics are not new. According to a research report prepared by Capital Link, a quarter of all California clinics had less than 30 days’ worth of cash on hand in 2019. But the pandemic, and the mass cancellations of office visits that accompanied it, wracked clinics almost immediately. Most of them rely on federal reimbursement for patient visits through Medi-Cal under guidelines set by the Health Resources and Services Administration, and traditionally that model paid only for in-person care.
The advent of telehealth is a path to reaching rural residents more quickly, but only if clinics can still receive payment for their services. Both California and the federal government, recognizing this, put waivers in place to allow for the reimbursement of telehealth visits at the same rate as in-person treatment. While that was a relief to many clinics operating on razor-thin margins, those working with rural patients quickly discovered another obstacle: Without widespread access to broadband internet, some areas couldn’t conduct telehealth visits anyway. And many clinics lacked the infrastructure — cameras, high-security computer systems and connections — needed to build a successful remote health system on the fly.
“It’s been one thing after another,” a clinic executive in rural Northern California told Capital & Main last month. “But the worst of it is right now, when we have vaccines on hand and can’t get people to take them. We knew the numbers were going to start going up.”
Reaching patients in far-flung and sparsely populated areas has long been a challenge, but in the time of COVID it has taken on a different sort of urgency.
According to data compiled by the Los Angeles Times, rural Northern California and the agriculture-heavy San Joaquin Valley have the two lowest collective vaccination rates in the state at 44% and 45%, respectively. Those regions also experienced some of the highest death rates from COVID over the summer: 33 per 100,000 residents in rural Northern California, 22 per 100,000 in the San Joaquin Valley. That compared with 13 per 100,000 in Southern California and just seven per 100,000 in the Bay Area, 70% of whose population is fully vaccinated.
Reaching patients in far-flung and sparsely populated areas has long been a challenge, but in the time of COVID it has taken on a different sort of urgency. Among other things, clinicians say, being in contact with a patient, whether in person or online, offers a chance not only to improve health but also to dissolve vaccine ignorance and dispel fears.
Melissa Marshall, CEO of six CommuniCare clinics in Yolo County, counts many farmworkers among the clinics’ patients. Earlier this year, with vaccines at the ready, she found that her staffers were battling two fronts: misinformation about the medicine itself, and fears by undocumented workers about their immigration status. (Vaccination in California is free and offered regardless of immigration status, according to the state.)
“It is slow going and a lot of work,” Marshall said. Her clinics pivoted hard toward telehealth, using grant funding until state and federal reimbursement measures kicked in.
* * *
It’s not clear what will happen in COVID’s wake. Congress has not yet signaled a desire to make telehealth reimbursement a permanent part of Medicaid, although doctors and health systems have reported strong patient interest in continuing to use telehealth as part of their overall care. The $550 billion infrastructure bill passed this summer by the U.S. Senate, meanwhile, includes $65 billion to expand broadband access across the country.
Improvements in both areas would work to the good of rural clinics and hospitals that have been grinding to continue reaching vulnerable communities and remote patients. In California as elsewhere, the stakes remain enormously high. A vital health clinic system needs to be made a priority for years to come.
Copyright 2021 Capital & Main

-
 Column - State of InequalityJanuary 22, 2026
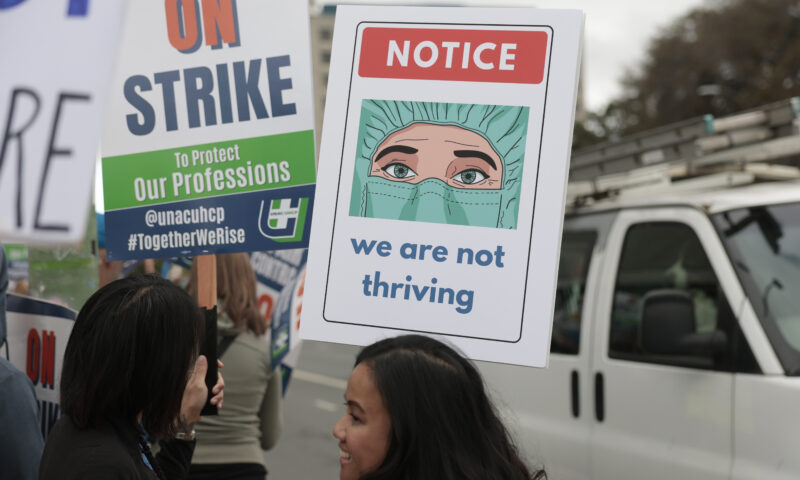
Column - State of InequalityJanuary 22, 2026On Eve of Strike, Kaiser Nurses Sound Alarm on Patient Care
-

 The SlickJanuary 20, 2026
The SlickJanuary 20, 2026The Rio Grande Was Once an Inviting River. It’s Now a Militarized Border.
-

 Latest NewsJanuary 21, 2026
Latest NewsJanuary 21, 2026Honduran Grandfather Who Died in ICE Custody Told Family He’d Felt Ill For Weeks
-

 The SlickJanuary 19, 2026
The SlickJanuary 19, 2026Seven Years on, New Mexico Still Hasn’t Codified Governor’s Climate Goals
-

 Latest NewsJanuary 22, 2026
Latest NewsJanuary 22, 2026‘A Fraudulent Scheme’: New Mexico Sues Texas Oil Companies for Walking Away From Their Leaking Wells
-

 The SlickJanuary 23, 2026
The SlickJanuary 23, 2026Yes, the Energy Transition Is Coming. But ‘Probably Not’ in Our Lifetime.
-

 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026The One Big Beautiful Prediction: The Energy Transition Is Still Alive
-

 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026Are California’s Billionaires Crying Wolf?

