Reinvesting in America
In North Carolina, the Uninsured Say Medicaid Expansion Will Be Life-Changing
After years of contentious battles amid a rural health crisis, the state voted to expand the program.

When Mike Dawkins’ mother Deanna learned she had cervical cancer in 2018, it was already stage 4. Several years before, the special ed teacher from Winston-Salem, North Carolina, had been taking medication to treat a thyroid condition when she learned she was pregnant. She was covered by Medicaid throughout her pregnancy, which is state policy.
Join our email list to get the stories that mainstream news is overlooking.
Sign up for Capital & Main’s newsletter.
“She carried the baby to term, but he was stillborn,” Dawkins explains. His mother was also diagnosed with fibroids, benign growths in her uterus. After delivery, Deanna no longer qualified for Medicaid and went without coverage. “She was in no shape to work,” Dawkins adds. His mom was deeply traumatized after the heartbreaking loss. Eventually, Deanna got a new job but didn’t qualify for insurance right away. It wasn’t long after that when she received the cancer diagnosis. Deanna Dawkins tragically died in 2020 at the age of 47, only two years after her diagnosis. When cancer is diagnosed early, the prognosis is much less grim, and patients can live longer and even go into remission. “Hers was just too far gone,” Dawkins explains.
Death, pain and at-home treatments like over-the-counter medications and herbal medicine were something many North Carolinians suffered through living in a state that has rejected Medicaid expansion — until this year.
In the years since President Obama signed the Patient Protection and Affordable Care Act (ACA), into law on March 23, 2010, 39 states and Washington, D.C., had embraced Medicaid expansion, enabling tens of millions of Americans to obtain health insurance.
North Carolina was one of the holdouts — the state has missed out on “an estimated $521 million each month that could go to improving mental health and helping rural hospitals stay open,” per a press release from Gov. Roy Cooper’s office — and, as a result, rural residents are 30%-40% more likely to be uninsured, according to Kody Kinsley, secretary of the North Carolina Department of Health and Human Services.
“Eighty percent of the uninsured in North Carolina are working families.”
~ Kody Kinsley, secretary, NC Department of Health and Human Services
On March 23, all that changed when the state House of Representatives voted 87-24 on a bipartisan basis, and North Carolina became the 40th state to approve Medicaid expansion. Despite strong political headwinds and conservative opposition, Gov. Cooper (D) persisted in leading state and local agencies and coalitions to advocate for expansion. Not only did the ACA create state health insurance exchanges to make private insurance affordable, but it also allows states to expand their Medicaid programs by raising the income limits to 138% of the federal poverty level. The federal government subsidizes the added costs to the states.
According to Secretary Kinsley, after Medicaid is expanded in 2023, a family of four in North Carolina could earn up to approximately $41,400 a year and remain eligible as opposed to approximately $8,900 before expansion.
“Eighty percent of the uninsured in North Carolina are working families,” says Kinsley. Some are single individuals working three jobs and don’t qualify for Medicaid but don’t make enough to afford insurance on the exchange. Now, thanks to expansion, at least 600,000 more adults in North Carolina will gain coverage through Medicaid. This is a huge win for North Carolina, with benefits that can be life saving and life changing.
But that epic transformation is not completely a done deal — when state lawmakers pushed it through, they added a condition that the state budget had to pass first before they can officially start the Medicaid expansion. The state budget cleared the state Senate on May 18, and negotiations are pending in the House.
Life or Death, and a Lot of Profound Pain
Evita B., a child care worker in the North Carolina Triangle area, is one of the many who will finally be eligible for Medicaid under expansion. She’s gone five years without coverage, ever since she was no longer eligible to stay on her mother’s health insurance policy after age 25. “I’ve had Aflac for a few years, and while it’s handy, it definitely doesn’t provide adequate coverage when really needed,” Evita explains. She was caught in the classic “gap,” earning too much for Medicaid but not enough for coverage on the health care exchange, better known as Obamacare. The sky-high premiums of private insurance were beyond her reach. Evita did her best, taking extra precautions when children in the day care were sick to avoid getting sick herself.
“I did everything I could to stay healthy and avoid a trip to the doctor or hospital,” she says, adding that she took vitamins and over-the-counter medications instead. Still, Evita accumulated a lot of medical debt from hospital visits, not to mention her dental issues. A few years ago, Evita began experiencing incredible tooth pain. “I scheduled an appointment, which cost me $245,” she says. After X-rays revealed she needed three wisdom teeth extracted and the cost would be more than $1,000, Evita held off on treatment and has been enduring constant tooth pain ever since. “Once I finally have Medicaid, it will be no more pain for me!” she explains.
A Hefty Price to Pay Without Expansion
For years North Carolina was stubbornly resistant to expansion due to partisan politics and conservative concerns that the federal government would change its mind and drop the financial assistance, which Republicans feared would bust the state budget. Instead, the assistance remains solid, with the feds picking up 90% of the tab. When Gov. Cooper took office in 2017, he began building bipartisan coalitions, which led to the historic vote. It took a diverse coalition of communities and businesses, and good old fashioned grassroots efforts from both sides of the aisle to gain overwhelming support to pass. “Because of all the noise constituents made, and the evidence showing that states that expanded Medicaid were doing better, the legislation finally passed,” says Ciara Zachary, PhD, MPH, an assistant professor at the University of North Carolina’s Gillings School of Global Public Health.
North Carolina has a significant rural population, and the impact of rejecting Medicaid expansion has been devastating in those areas. “We had seven rural hospitals close in nearly 10 years,” says Kinsley. “We’ve been paying for all of this [health care] only in the most expensive way possible. Penny-wise and pound-foolish.”
Mark Beamer, a family medicine physician at ECU Health Multispecialty Clinic in Belhaven, is especially concerned about the state of rural health care, the impact of which he sees every day in this waterfront town in Beaufort County.
In Belhaven, Pungo Hospital was shut down by Vidant Health in 2014.
When hospitals close, people leave, and businesses close their doors. It’s a vicious cycle that makes it extremely difficult for remaining residents to get medical care.
“Anytime a hospital closes in a community, there is understandably going to be some uncertainty and some hurt,” Beamer explains. “The community in and around Belhaven was certainly no different, and we, as health care providers, feel that concern.” For years, patients were used to being able to visit the hospital to receive services like transfusions and X-rays, and now they must travel farther and sometimes wait longer for care. “I will say that we are fortunate to be connected to a system of care,” Beamer adds. “Some communities get left behind altogether when a hospital closes.” The services at ECU Health Multispecialty Clinic meet important health care needs in the community, but rural providers have had to think differently about how to provide care.
Eastern North Carolina has a disproportionate number of chronic diseases like hypertension and diabetes when compared to the rest of the state — and these patients show up in the emergency room with advanced and complex conditions that require more time, energy and resources to treat, says Leigh Patterson, chief of emergency services at ECU Health Medical Center Hospital in Greenville. They are uninsured or underinsured and have no access to primary care. “This strains the Emergency Department and creates longer wait times for patients,” Patterson explains, adding that many uninsured seek out the ED as a means of receiving primary care. Without adequate insurance coverage, it’s more challenging to arrange follow-up visits and ensure patients have access to medications they need. “This can result in patients ultimately being admitted into the hospital to receive care they otherwise could have received in the outpatient setting,” Patterson adds.
Zachary adds that when hospitals go under due to financial strain from providing uncompensated care, a ripple effect occurs that launches the dreaded “brain drain.” “People tend to work where they live,” she explains. When hospitals close, people leave, and businesses close their doors. It’s a vicious cycle that makes it extremely difficult for remaining residents to get medical care.
According to Jamal Jones, the chief administrative officer at Piedmont Health Services, a federally qualified health center in Raleigh, Medicaid expansion will help reduce the numbers of uninsured and help health care centers stay afloat, extend outreach and serve patients in counties where many working poor and underserved live.
Generous Financial “Sweetener” Will Help Mental Health and Persistent Health Disparities
What turned the tide in North Carolina and swayed the minds of legislators was the promise of a fiscal bump from the American Rescue Plan to the tune of an extra $1.8 billion, a “signing bonus” for states that expand. “The money will come to North Carolina in eight quarterly payments over two years,” Kinsley explains, which will help fund behavioral health services.
“This is the new crisis,” Kinsley says, adding that the lack of behavioral health services worsens the opioid crisis. “It touches every community and every family.” Drug overdoses are on the rise in North Carolina, as in much of the country. “We had sheriffs from rural communities saying that they can’t arrest their way out of a mental health problem,” Kinsley says. He is hopeful expansion will also address pervasive health disparities affecting the African American and Native American populations that have plagued the state for years. Also hopefully to be addressed is the rising maternal mortality rate: In North Carolina, Black infants are twice as likely to die, and Black mothers are three times more likely to die, than their white counterparts. Even with the Medicaid program for pregnant women, disparities persist. Preventive care is lacking. “Women have to be well before they even get pregnant,” Kinsley explains.
A Looming Sense of Urgency to Preserve Continuity of Patient Care
The clock is ticking due to another complication. During the pandemic, the federally mandated COVID-19 Public Health Emergency (PHE) meant no one was disenrolled from Medicaid, while the usual process to redetermine eligibility was paused for three years. But the PHE expired on May 11, redetermination has started again, and people will have to submit income documentation to see if they still qualify. Some will lose their Medicaid coverage because their income is too high pre-expansion, and will have to reapply when expansion is allowed to begin.
“We must get the budget passed. We have people that expansion can rescue from losing their coverage,” Zachary urges. Kinsley says agencies are warming up the engines, getting eligibility workers trained, and working with the federal government on policy issues. “We’re getting all the train cars lined up and as soon as the budget passes, the train can leave the station,” Kinsley says. It’s imperative to prevent any interruption in the continuity of patient care. “We don’t want these individuals dropping off Medicaid, stopping their medications, and not being able to see their doctors.”
Already, many in the state are losing Medicaid, and the process of reapplying can take a while. It’s more costly for both patients and the system to start back at square one, and it’s twice as much work for state eligibility workers getting people back on again.
“One thing we learned during the pandemic is that we can build the plane while going down the runway.”
~ Jamal Jones, chief administrative officer, Piedmont Health Services
“By expanding access to health insurance through Medicaid expansion, patients can receive early treatment in the primary care setting, helping them better manage their conditions and reducing the likelihood of an Emergency Department visit and an unplanned admission,” Patterson says.
Some advocates question the wait, especially with the end of the PHE, which will dump roughly 370,000 North Carolinians off Medicaid, and more than 100,000 of those are expected to qualify under Medicaid expansion, according to Zachary.
“[After expansion] Emergency Department team members will be able to refer uninsured patients to the Department of Social Services or Access East, the care management arm of ECU Health, to connect them with Medicaid resources,” Patterson says.
Jones says his staff at Piedmont Health Services has been notifying patients about their redetermination dates and checking Medicaid eligibility when they come for a visit. Redetermination, the process of reapplying and providing updated income information, for the traditional Medicaid population, is generally done by county social services and will be processed by social services as their redetermination month rolls around.
New enrollment determinations for the expansion population are expected to shift to the federal marketplace. Jones remains optimistic. “One thing we learned during the pandemic is that we can build the plane while going down the runway,” Jones says, giving all the credit to his team and staff members for quick thinking and agility navigating unprecedented, uncertain times. “They had it all figured out,” Jones says, “And we are prepared to figure [expansion] out as we go along.”
Meanwhile, North Carolinians are waiting. “This expansion is life-changing for me,” Evita says. “You truly never know how much you appreciate the small things until they are no longer accessible,” she explains, “I don’t plan to get sick anytime soon, but having the peace of mind knowing that I’m covered is what I’ve longed for.”
Copyright 2023 Capital & Main

-
 Column - State of InequalityJanuary 22, 2026
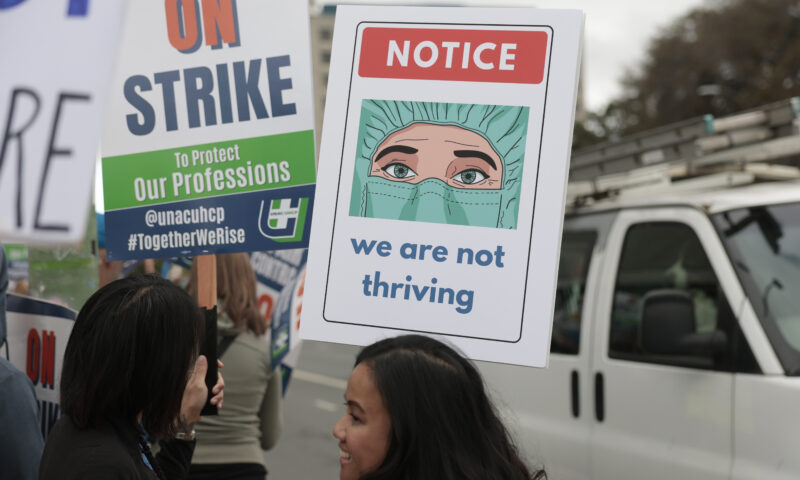
Column - State of InequalityJanuary 22, 2026On Eve of Strike, Kaiser Nurses Sound Alarm on Patient Care
-

 Latest NewsJanuary 21, 2026
Latest NewsJanuary 21, 2026Honduran Grandfather Who Died in ICE Custody Told Family He’d Felt Ill For Weeks
-

 Latest NewsJanuary 22, 2026
Latest NewsJanuary 22, 2026‘A Fraudulent Scheme’: New Mexico Sues Texas Oil Companies for Walking Away From Their Leaking Wells
-

 The SlickJanuary 23, 2026
The SlickJanuary 23, 2026Yes, the Energy Transition Is Coming. But ‘Probably Not’ in Our Lifetime.
-

 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026The One Big Beautiful Prediction: The Energy Transition Is Still Alive
-

 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026Are California’s Billionaires Crying Wolf?
-

 Latest NewsFebruary 3, 2026
Latest NewsFebruary 3, 2026Amid the Violent Minnesota Raids, ICE Arrests Over 100 Refugees, Ships Many to Texas
-

 Dirty MoneyJanuary 30, 2026
Dirty MoneyJanuary 30, 2026Amid Climate Crisis, Insurers’ Increased Use of AI Raises Concern For Policyholders

