Reopening the Golden State
Safety Unknowns Await Returning Medical and Dental Workers
Hospitals and clinics that recently faced financial collapse are reopening waiting rooms. But PPE shortages and staff-risk issues remain.

In late April, as medical offices around California closed down to all but emergency and COVID-19 patients, staff at the hospital and clinics run by Stanford University were told they would be furloughed one day a week through at least late June to save the hospital money during the outbreak. Stanford argued its “temporary workforce adjustment” was utilizing paid time off for workers — essentially encouraging workers to take vacations and paid sick leave — in order to preserve Stanford’s workforce over the long term and keep its workers’ earnings largely intact in the short term.
Steve Trossman, a spokesman for SEIU-United Healthcare Workers West, the union that represents nearly 2,500 of the Stanford University Medical Center workers, says it was one of the first hospitals in California in which the SEIU has a presence to aggressively move to curtail workers’ wages during the COVID-19 crisis. At the time, hospital incomes were cratering due to their inability to see patients for lucrative non-emergency procedures and consultations.
Today, at the back end of the shutdown, workers are coming back into environments they fear have been rendered less safe both by the epidemic and by the cuts in staffing that accompanied it.
Around the state and the country, medical centers confronted huge, rapid collapses in their fiscal situations. Stanford wasn’t alone in battening down its financial hatches. Nor has it been alone in finding that, at the back end of the shutdown, workers are coming back into environments they fear have been rendered less safe both by the epidemic itself and by the cuts in staffing that accompanied it.
The California Primary Care Association (CPCA), says its president, Carmela Castellano-Garcia, calculated that more than 205 of California’s 1,300 federally qualified clinics — which serve up to 7 million low-income and immigrant Californians — shut their offices at the start of the crisis, meaning that poor, mainly immigrant patients either had to travel further for treatment or had to make do with phone visits with doctors in lieu of in-person exams. The same conditions spread to more mainstream hospitals large and small. Doctors, from psychiatrists to kidney specialists, moved an increasing number of appointments into the realm of telemedicine, buoyed by the federal and state slashing of red tape that allowed Medicare, Medicaid and other insurance systems to fully reimburse doctors for telemedicine appointments.
Meanwhile, optometrists, physical therapists and other “hands-on” specialists all stopped seeing their routine appointments. Most of the state’s approximately 36,000 dentists had to massively cut back their in-person visits with patients, according to Dr. Judee Tippett-Whyte, the Stockton-based president-elect of the California Dental Association.
And as the lights went out in waiting rooms everywhere, many of the in-office support staff who normally assist patients found their services no longer needed and were laid off. Now, in June, with elective surgeries and other non-emergency procedures resuming as the state begins to reopen, staff worry that these workplace cuts mean that the employees on hand will be asked to do more with less — resulting in potential health risks to patients and medical personnel alike.
With elective surgeries and other non-emergency procedures resuming as the state begins to reopen, staff worry that workplace cuts made early in the pandemic mean that the remaining employees will be asked to do more with less.
“We have to do eight hours [of work] in seven hours,” claims Linda Cornell, a 72-year-old medical unit secretary on an organ-transplant unit at the Stanford hospital. She works the nursing station answering call lights from patients, doing paperwork, retrieving medications to give to patients at the right time each day and dispatching nurses to assist patients in need. “I consider myself the air traffic controller of the unit.”
But now, she says, as she and her staff ramp up for a full patient load again, “I worry about the patients not getting help in time. I typically work four days a week; now I’m cut back to three. [Before the lockdown] our housekeepers might have an entire floor.” Today, however, those housekeepers may have to cover three or four additional floors with no additional help: “Things don’t get done. It may be hours before you get isolation trash removed from a patient’s room.”
Read Other Stories From This Series
Julie Greicius, a communications spokesperson for Stanford Health Care, which operates the university’s hospital system, denied these allegations: “No employees were required to take on additional work,” she wrote in an email response. “Responding to a decrease in patient volumes as a result of preparation for a possible surge in COVID-19 patients, the Temporary Workforce Adjustment allowed us to match our daily workforce to demand across the organization.”
* * *
So worried are some of the workers at Stanford University Medical Center that, Cornell alleges, nurses have written up SAFE reports, detailing conditions that, they claim, jeopardize patient well-being. She was present, she says, when one nurse discussed a report alleging that trash and dirty linen was left for hours in the isolation room of a patient because of staff shortages. Even more worryingly, Cornell says, producing a memo from the hospital to back up her claim, “they’ve reduced the lab draw personnel, so now the nurses have to do a large proportion of lab draws, which they routinely don’t do. The lab personnel do it all day long; the nurses aren’t as good at it. They may have to poke a patient several times to get it done. They’ve cut back on transports, so patients are delayed getting to procedures and to tests.”
But it’s not only patient safety that concerns her. She claims the hospital never indicated during the lockdown that Cornell, who is in a medically vulnerable age group, could stay away from work if she felt she needed to. Similarly, she says, fellow workers who are diabetic or have other conditions that put them in high-risk categories have also had to work through the pandemic.
“The shortage of PPE is real, and hospitals are struggling to figure out how to make enough masks go further.”
— Union spokesman
While Stanford Health Care argues that it did offer immune-compromised workers, and workers with underlying health conditions, what it calls “alternate work assignments,” Cornell says that she and her co-workers weren’t given such options.
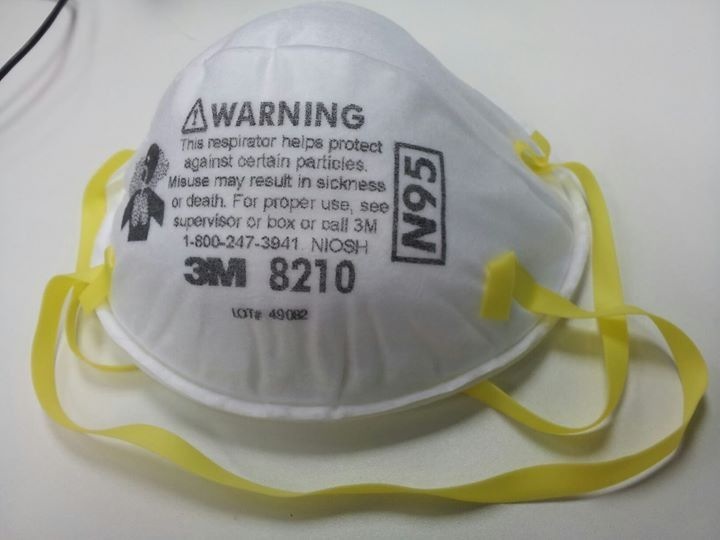
Now, with the pandemic still raging, Cornell and her colleagues are concerned that they don’t have adequate personal protective equipment (PPE) to keep them safe as they start engaging with more patients again.
“We get one mask a day,” explains Cornell. “Currently, we are rationing our masks, saving them to be recycled. They’re supposed to do some kind of sanitization process. A lot of us are kind of nervous. In normal times, you’d use one new, clean mask every time you enter the room, and then you’d dispose of it.”
(Editor’s Note: Stanford Health Care asserts that it does not limit its workers to one mask a day.)
Moreover, cleaners, transporters and other nonmedical staff have told Cornell’s union that they are routinely denied N95 masks, and are being asked to clean rooms in which COVID-19 patients have stayed, without the recommended 24-hour gap between when a patient leaves and when a cleaner comes in.
Similar stories are playing out up and down the state. “The shortage of PPE is real, and a number of hospitals are struggling to figure out how to make enough masks go further,” says SEIU’s Trossman.
* * *
Perhaps in no area of medicine has the PPE shortage emerged as more of a problem than in dentistry, where personnel working in close proximity to patients’ open mouths are exposed to particular hazards during an outbreak of a respiratory virus passed along by aerosolized droplets exhaled by those with the disease.
Last March Dr. John Blake and his 17 fellow dentists at the Long Beach Children’s Dental Health Clinic stopped seeing all patients but those with the most severe emergencies. “We were down to a skeleton crew,” says Blake. “One dental assistant, some front-office staff,” with Blake himself as the resident dentist.
As financially fragile clinics and medical centers ramp up to maximum patient caseloads again, the stresses on the system — and the potential for staff to be placed at risk — will only intensify.
Not needing their supplies of PPE since they weren’t seeing as many patients, Blake and many other dentists around the state donated urgently needed N95 masks and other protective gear to hospitals, hoping they would have ample time to restock before they saw patients again.
Now, Blake is trying to navigate the complex path that leads to reopening. He has to hew to guidelines put out by the American Dental Association, by the California Dental Association (CDA), by the State of California and by Los Angeles County. Sometimes the guidelines complement each other; at other times, they contradict each other — and if the county and the state guidelines don’t mesh, it’s the most restrictive ones that must be adhered to.
“We set up an initial triage area” in the office, he explains. “My front office staff is in full PPE. We warn the patients it’ll look different. They have their temperature taken and another symptoms review. Then they are checked in.”
Although this ensures a safer environment, it also means that Blake’s dental office is seeing fewer patients per day than it used to, resulting in his clinic having less revenue coming in to sustain operations, just at a time when it’s costing ever more to secure PPE supplies. And that falloff in revenue risks contributing to a downward spiral in which medical offices lay off workers, patients have to wait longer for appointments and those workers who have kept their jobs find they are having to perform more roles in the office than they did previously.
As for securing PPE, some dentists report having to scavenge for masks — with N95s going for up to $7 each — hair coverings, face shields and foot coverings in a market in which their competitors include big hospital chains, state governments and the Federal Emergency Management Agency (FEMA). Others, says Dr. Tippett-Whyte, even report buying masks only to have FEMA confiscate the supplies while they are en route to their offices. Tippett-Whyte also notes that other CDA members have resorted to buying masks on the black market only to find, once they arrive, “that they are junk.”
As financially fragile clinics and medical centers around the state ramp up to maximum patient caseloads again, the stresses on the system — and the potential for staff to be placed at risk — will only intensify. In late May, Carmela Castellano-Garcia of the CPCA estimated that 90 percent of California’s federally qualified health clinics were reporting that they currently had enough PPE supplies for their staff. But, she said, that was only because they were still working at extremely limited capacity. “They’re concerned about next month,” she acknowledged, “when they’re bringing back workers who have been furloughed and when dental clinics open up.”
“We’re starting to get back to work,” says 58-year-old dental assistant Shari Becker, who works in Danville, in Contra Costa County. But, she says warily, “my goodness, it was a shock and it is a shock. To the whole community. The unknowns. We’re just at the tip of the iceberg.”
Copyright 2020 Capital & Main

-

 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026The One Big Beautiful Prediction: The Energy Transition Is Still Alive
-

 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026Are California’s Billionaires Crying Wolf?
-

 Latest NewsFebruary 3, 2026
Latest NewsFebruary 3, 2026Amid the Violent Minnesota Raids, ICE Arrests Over 100 Refugees, Ships Many to Texas
-

 Dirty MoneyJanuary 30, 2026
Dirty MoneyJanuary 30, 2026Amid Climate Crisis, Insurers’ Increased Use of AI Raises Concern For Policyholders
-

 Featured VideoFebruary 4, 2026
Featured VideoFebruary 4, 2026Protesters Turn to Economic Disruption to Fight ICE
-

 The SlickFebruary 2, 2026
The SlickFebruary 2, 2026Colorado May Ask Big Oil to Leave Millions of Dollars in the Ground
-

 Column - State of InequalityFebruary 5, 2026
Column - State of InequalityFebruary 5, 2026Lawsuits Push Back on Trump’s Attack on Child Care
-

 Column - California UncoveredFebruary 6, 2026
Column - California UncoveredFebruary 6, 2026What It’s Like On the Front Line as Health Care Cuts Start to Hit