Coronavirus
L.A. Public Health Ok’d Release of COVID Patients to Nursing Homes With Many Coronavirus Deaths, Poor Ratings
The agency also scrubbed statistics on coronavirus deaths and cases at designated nursing homes from its website.
As part of California’s controversial practice of discharging COVID-19 patients from acute-care hospitals into nursing homes, L.A. County’s Department of Public Health (LAC DPH) has designated 21 facilities to accept people with the disease caused by the coronavirus. But data reviewed by Capital & Main show that at least 240 residents of these facilities have died of COVID-19, and that most of the nursing homes approved by public health officials to take COVID-19 patients have poor overall ratings, higher-than-average health deficiency levels and low staffing.
The findings raise questions about whether residents already living in these facilities are being exposed to the potentially deadly virus by discharged COVID-19 patients, and how or whether the agency is vetting facilities before allowing them to accept those recovering from the disease.
“LAC DPH’s decision to promote by listing on their website problematic facilities that were willing to accept COVID-19 patients was an act of desperation,” said Dr. Noah Marco, chief medical officer at the Los Angeles Jewish Home, in a statement sent to Capital & Main. “Desperation created by not enlisting the advice offered to them by experts in long-term care, and not appropriately anticipating the easily predictable devastation that is occurring in L.A. County nursing facilities.”
Among the 21 facilities approved by LAC DPH to take COVID-19 patients from hospitals, eight have seen 13 or more resident deaths related to the disease: 28 at Grand Park Convalescent Hospital, 22 each at Alden Terrace Convalescent Hospital and Kei-Ai Los Angeles Healthcare Center, 21 at Monrovia Gardens Healthcare Center, 19 at Country Villa South Convalescent Center, 15 at Sunray Healthcare Center and 13 each at Country Villa East Nursing Center and Lynwood Healthcare Center, according to data from the California Department of Public Health.
* * *
Capital & Main has also learned that the L.A. County Department of Public Health has removed 20 of the 21 facilities designated to take COVID-19 patients from its website page that lists COVID-19 cases and deaths for all nursing homes in L.A. County. A list obtained by Capital & Main documents COVID-19 deaths at the 20 LAC DPH-approved facilities that no longer appear on the agency’s website. The data from that list reflect COVID-19 fatalities prior to the removal of the nursing homes from LAC DPH’s website. The removal of this information makes it difficult for the public to know how these facilities have been affected by the pandemic, and has alarmed advocates for nursing home residents.
“It’s disgraceful that L.A. County Public Health is keeping the public in the dark about the deadly outbreaks that have taken place in these designated COVID-19 facilities,” said Connors of California Advocates for Nursing Home Reform. “Whitewashing their outbreak histories is every bit as appalling as designating such dangerous places to serve COVID-19 patients.”
Charlene Harrington, professor emeritus at the University of California, San Francisco, and an expert on nursing home reform, told Capital & Main that taking the facilities off the website reduces their transparency and accountability. “They should have to report like every other nursing home in the state — there is no excuse for L.A. County to remove them. It is deceptive to the public.”
In an email, Capital & Main asked LAC DPH’s media department where a list could be found of COVID-19 cases and deaths at county nursing homes approved by the agency to accept patients with the disease. LAC DPH directed a reporter to the state’s website. That site has incomplete information, and is not listed as a resource in the section of LAC DPH’s webpage on COVID-19 cases and deaths at county nursing homes.
Capital & Main reviewed data on nursing home ratings, staffing and health deficiencies from the Centers for Medicare and Medicaid Services. Among the 21 facilities approved by LAC DPH to accept COVID-19 patients from hospitals, eight have a rating of only 1 or 2 on the federal government’s 5-point scale. On adequate staffing levels — a critical factor in infection control — the 21 facilities have an average rating of 2.25 on the 5-point scale, with 15 nursing homes ranking at 1 or 2 stars. The overall staffing rating for registered nurses (RNs) is 1.95, with 15 of the 21 facilities ranking at 1 or 2 stars. Only one meets the minimum daily number of hours per resident for certified nursing assistants recommended by experts, and none meet the recommended daily minimum of hours per resident for registered nurses. The facilities also have a 36 percent higher level of health deficiencies than the average California nursing home.
“Instead of selecting high-quality facilities, L.A. County allowed many facilities with low quality and low staffing to become designated,” wrote Harrington in her email. “It was clear from the beginning of the pandemic that nursing homes’ residents were highly vulnerable to COVID infections. Once the COVID virus was introduced into nursing homes it spread wildly because most nursing homes did not have adequate RNs, who are the primary ones to implement and oversee infection control.”
In a statement, LAC DPH told Capital & Main that skilled nursing homes are self-designating to accept COVID-19 patients, and that the appearance of these facilities on the agency’s website does not constitute a county endorsement. But the department’s site states that facilities must be approved by LAC DPH after submitting a plan for how they will keep patients safe.
In a May 5 email to Dr. Michael Wasserman, president of the California Association of Long-Term Care Medicine, Dr. Zachary Rubin of LAC DPH’s Acute Communicable Disease Control Program wrote, “When we are approached by facilities to consider being designated as a COVID care site, we have a team vetting these requests to ensure the safest possible situation for patients who have unique needs while recovering from COVID-19.” LAC DPH did not respond to questions about their vetting process or criteria.
The first nursing home to start accepting COVID-19 patients in L.A. County was Country Villa South — which was also the site of one of L.A. County’s first deadly COVID-19 outbreaks. The facility has a record of recent infection control violations, and a one-star rating. “It’s outrageous that the County is designating nursing homes that have been death traps during this pandemic to be dedicated COVID-19 facilities,” said Michael Connors with California Advocates for Nursing Home Reform in an emailed statement.
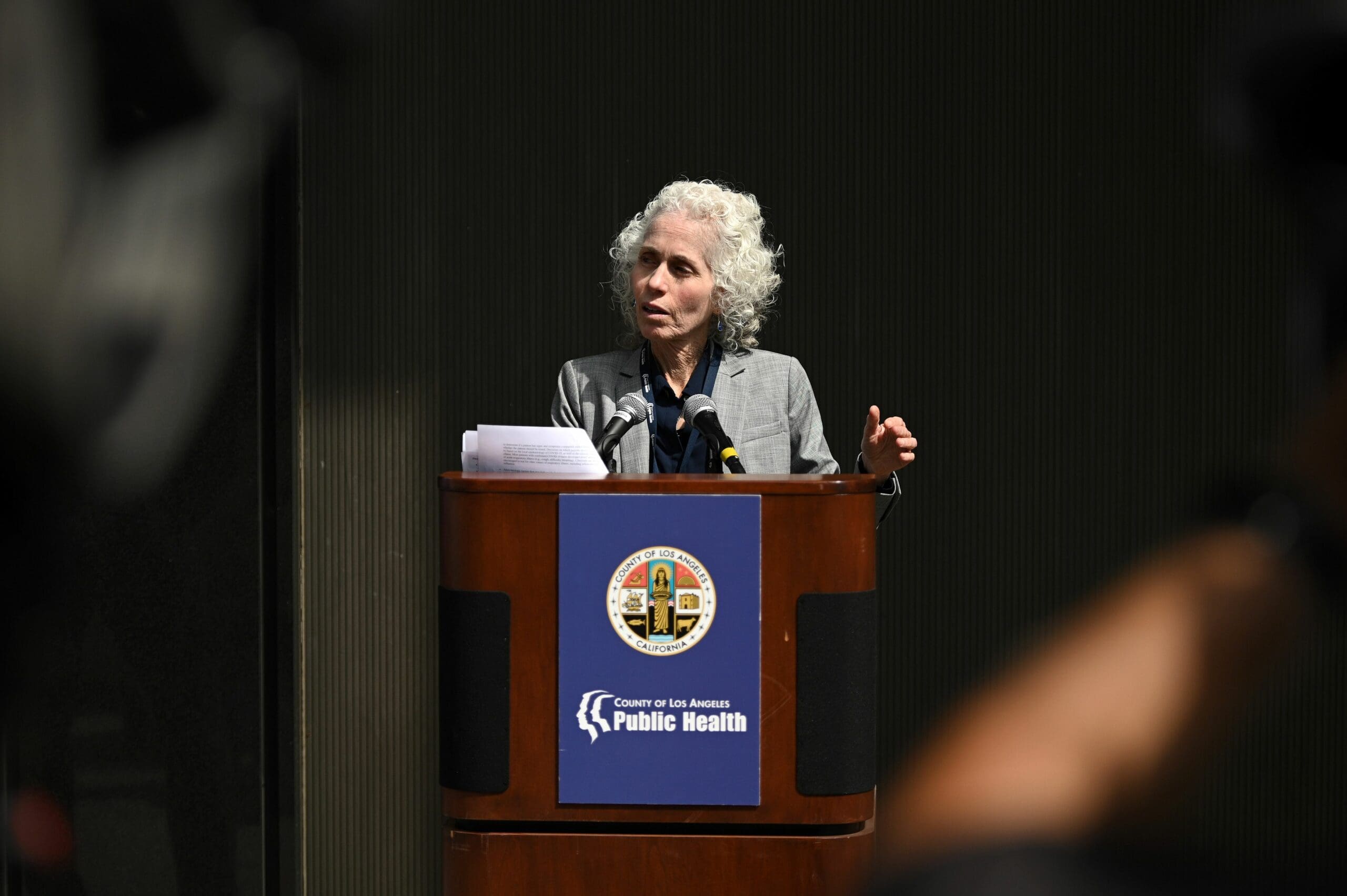
The decision by LAC DPH to allow facilities with poor track records to accept COVID-19 patients is only one example of how the agency has mishandled the viral outbreak at nursing homes in Los Angeles. A Capital & Main investigation found that, under the leadership of director Barbara Ferrer, LAC DPH failed to respond adequately as COVID-19 spread at skilled nursing facilities, which account for more than 1,400, or nearly 50 percent, of the county’s COVID-19 deaths. Ferrer did not respond to interview requests for that investigation.
A former senior manager at LAC DPH, who requested anonymity, questioned the competence of Ferrer to lead the department and remarked in a statement to Capital & Main, “The decision to approve these facilities is a recipe for disaster: poor ratings, histories of repeated operational deficiencies, inadequate numbers of professional nursing staff and not enough overall staff to provide care for COVID patients. It is unconscionable that L.A. County could conclude that this would be even ‘adequate care’ for our elderly.”
Copyright 2020 Capital & Main

-

 Column - State of InequalityFebruary 5, 2026
Column - State of InequalityFebruary 5, 2026Lawsuits Push Back on Trump’s Attack on Child Care
-

 Column - California UncoveredFebruary 6, 2026
Column - California UncoveredFebruary 6, 2026What It’s Like On the Front Line as Health Care Cuts Start to Hit
-

 The SlickFebruary 10, 2026
The SlickFebruary 10, 2026New Mexico Again Debates Greenhouse Gas Reductions as Snow Melts
-

 Latest NewsFebruary 12, 2026
Latest NewsFebruary 12, 2026Trump Administration ‘Wanted to Use Us as a Trophy,’ Says School Board Member Arrested Over Church Protest
-

 Latest NewsFebruary 10, 2026
Latest NewsFebruary 10, 2026Louisiana Bets Big on ‘Blue Ammonia.’ Communities Along Cancer Alley Brace for the Cost.
-

 Column - State of InequalityFebruary 12, 2026
Column - State of InequalityFebruary 12, 2026They’re Organizing to Stop the Next Assault on Immigrant Families
-

 The SlickFebruary 16, 2026
The SlickFebruary 16, 2026Pennsylvania Spent Big on a ‘Petrochemical Renaissance.’ It Never Arrived.
-

 The SlickFebruary 17, 2026
The SlickFebruary 17, 2026More Lost ‘Horizons’: How New Mexico’s Climate Plan Flamed Out Again

