Battery Blood
Battery Blood: How California Health Agencies Failed Exide Workers
California’s Department of Public Health and Cal/OSHA didn’t protect workers from lead contamination at a battery recycling plant. A state Assembly member will hold hearings for a worker-protection bill based on our investigation.

Even as health agencies in other states issued six-figure fines and ordered multimillion-dollar safety improvements of battery recycling plants, California’s enforcement was strangely anemic.
For nearly a century a hulking industrial plant near downtown Los Angeles melted down car batteries to reclaim their lead. The facility, most recently owned by Exide Technologies, was shut down in 2015 in a deal the company made with the U.S. Justice Department to avoid criminal prosecution for polluting nearby residential communities. Neighborhood activists have criticized California’s Department of Toxic Substances, which allowed Exide to continue operating for years with a temporary permit, despite evidence it was a major polluter. But a year-long investigation by Capital & Main and the University of Southern California’s Center for Health Journalism has found that two other agencies, the California Department of Public Health (CDPH) and the Division of Occupational Safety and Health (Cal/OSHA), failed to take action during a simmering public health crisis involving hundreds of lead-poisoned workers at the plant.
Between 1987 and 2014, according to records we obtained from CDPH, California health officials were aware of more than 2,300 blood tests from the plant’s workers revealing blood-lead levels above 25 micrograms per deciliter — high enough to cause miscarriages, tremors, mood disorders and heart disease. While CDPH lacks the power to levy fines or mandate changes, it may refer cases to Cal/OSHA, which has that authority. But except for one fleeting moment in 1996, the agencies have operated in virtual silos, failing to coordinate actions or share incontrovertible evidence that the facility was a potential death trap.
“It’s distressing to know that Exide workers were exposed at that level and chronically,” said Dr. Bruce Lanphear, a physician and leading lead researcher with Simon Fraser University in Vancouver, Canada. “We’ve known for decades that lead at those levels can lead to hypertension and chronic renal failure [kidney disease]. California regulators were aware of this information and should have better protected these workers.”
In contrast to the anemic enforcement by California officials, regulators in much of the rest of the nation have, thanks to a strict federal lead directive issued in 2001, cracked down on perilous battery recycling plants — issuing six-figure fines and requiring multimillion-dollar safety improvements. Although the federal lead directive is legally binding in states where workers are directly protected by federal OSHA and eight other state-run programs that adopted these standards, California, the nation’s most populous state, never embraced them.
Exide appealed a $280 Cal/OSHA fine. It was ultimately reduced to $150 — less than the cost of a speeding ticket.
Despite California’s seemingly lower standards, Cal/OSHA told Capital & Main that “Cal/OSHA’s program is required to be, and is, at least as effective as federal OSHA.” However, despite hundreds of workers who developed lead poisoning at the plant, the only fine specifically related to lead that we found issued by Cal/OSHA at the site, which recycled about 25,000 lead-acid car batteries a day, was a 2008 citation for $150 — less than the cost of a speeding ticket.
The lead problem at the Vernon plant, which was acquired by Exide in 2000, goes back a long time. In the 1970s Jim Dahlgren, today a retired physician, treated 120 severely lead-poisoned workers from the plant, then owned by National Lead, and helped qualify them for disability insurance. Dahlgren, who worked for the University of California, Los Angeles, at the time, claimed that nearly all of those men died prematurely from complications due to lead exposure and that several patients fell into lead-induced comas. Dahlgren said his patients’ blood levels routinely measured above 100 micrograms per deciliter (μg/dL), a potentially lethal level. “Every single organ system of the body is impacted adversely by lead,” Dahlgren said. “These men had symptoms that ran the spectrum — severe abdominal pain, vomiting, diarrhea, palpitations, chest pains, trouble thinking, headaches.”
Read Documents Related to This Story
Dahlgren’s account was echoed in a 1973 Los Angeles Times article headlined “Plant Fumes Poisoning Plant Workers, Union Chiefs Say,” and an obscure 1976 documentary, Lead Smelter, which interviewed Dahlgren, along with gaunt, bedridden workers and their families.
Luis Rodriguez, a poet and writer who achieved fame with his memoir about escaping gang life, “Always Running, La Vida Loca, Gang Days in L.A.,” spent six months in 1978 working in the Vernon plant as a smelter. The plant’s huge furnaces melted down car batteries and separated out the lead into what is called slag.
“After you use the furnace, all the lead would fall to the bottom and there was a hole in the back called a slag hole,” Rodriguez said. “I had to use a jackhammer to hammer it open, and pull the slag out and put it into carts. A good friend of mine said, ‘You know you got to get out of there. Lead will kill you and your family.’ That woke me up, might have saved my life.”
California Department of Public Health warnings about the Vernon plant, which Exide Technologies purchased in 2000, took on the look of an annual form letter.
The CDPH declined interview requests or to answer specific questions by email, and instead issued a statement that read in part, “CDPH takes seriously any incidents that may affect the public health of the people in California,” adding that “there are always lessons to be learned, especially in the case of long-running complex community public health issues.”
Exide’s lead-poisoning problem, however, was well known to state officials. Because battery recycling involves potentially lethal exposure to lead, the company was required to test workers’ blood several times per year and to report the results to the CDPH. (Exide did not respond to emails and phone messages requesting comment.)
Despite the fact that CDPH was aware of more than 2,300 concerning blood lead tests among workers at the Vernon site, our investigation found that CDPH referred the company to Cal/OSHA only a few times in the 1990s, and that between 1990 and 2013, inspections of the plant related to lead by Cal/OSHA occurred only in 1995, 1996 and 2008. Records we obtained show the 1995 inspection was triggered by a complaint to Cal/OSHA from a private physician who had treated a plant worker with symptoms of lead poisoning and alarming blood-lead levels. Cal/OSHA determined “no serious injuries or illnesses detected” and issued no fines. The company, according to the inspection report, also told Cal/OSHA that “engineering controls were not feasible at the plant.”
By then the plant had changed hands and was owned by GNB Technologies. Despite the new ownership, lead poisoning among workers was still a huge problem. Blood-lead testing tracked by CDPH showed that in 1995, 135 workers at the site that year had seriously elevated levels of lead in their blood, and 33 workers had blood-lead levels above 40 μg/dL.
The same year Cal/OSHA’s inspection report dismissed concerns about fundamental safety at the plant, CDPH was expressing extreme concern. In 1995 CDPH’s Occupational Lead Poisoning Prevention Program chief, Barbara Materna, wrote a letter to GNB’s regional director, David Wesley, noting that the Vernon workers had blood-lead levels high enough to cause “increased blood pressure, damaged sperm, and impaired learning ability in children exposed to lead during pregnancy.” CDPH also expressed grave concerns that airborne levels of lead found in parts of the plant were more than 50 times above federal safety standards.
By 1996 CDPH had had enough. “Our policy is to work cooperatively with those who are improving health and safety conditions in their workplace,” Materna wrote GNB. “However, if serious conditions are not addressed in a timely manner we are obligated to make referrals to Cal/OSHA for enforcement actions.”
Capital & Main spoke to Mariano Kramer, then a Los Angeles-area Cal/OSHA district manager, who CDPH sent the referral letter to. In 1996, after receiving a referral from CDPH, he supervised the only inspection we could find that appears to have had any teeth behind it.
Former Cal/OSHA Manager: “The agency is a battleground between those who see the prime directive as protecting workers and others who are fearful of hurting the bottom line of industry.”
Cal/OSHA told us it was unable to locate records related to the 1996 inspection. Kramer recalls the case vividly, however: “It was a very messy situation at the plant and a lengthy process. We required them to make substantial safety improvements.” The fines and required safety upgrades, which Kramer said were levied, seemed to make a difference at the plant. Lead poisoning cases dropped 25 percent the following year.

Photo: Joanne Kim
However, the monitoring of the Vernon plant, which Exide Technologies purchased in 2000, became less frequent and appears to have amounted to an annual form letter. In 2005 CDPH told Exide, “We recently received one or more reports of elevated blood-lead levels at or above 40 μg/dL for employees of Exide Technologies.” The letter continued, “Elevated BLLs indicate serious problems with your lead safety program that should be corrected. They may also indicate violations of the Cal/OSHA Lead Standard.”
By then, according to records provided to Capital & Main by CDPH, about 40 workers per year continued to show alarming levels of lead in their blood. It wasn’t until 2008 that Cal/OSHA performed a new lead-safety inspection at the site. The inspection stemmed from an anonymous complaint from an Exide worker, and the inspectors don’t appear to have been armed with any of the information collected by CDPH. When inspectors arrived at the sprawling Vernon plant, records show, they took just one swipe of a surface in search of evidence of lead dust. The sample was taken on a shelf next to a telephone — in an office that was designated a lead-free zone, where workers were supposed to be able to take breaks without wearing any protective equipment. While the shelf had lead levels far in excess of federal standards, Cal/OSHA fined Exide just $280 for the safety violation it labeled “low” in severity. Exide appealed the fine and the violation was ultimately reduced to $150.
Cal/OSHA appeared even less concerned with the toxic air to which workers were exposed in the plant’s smelting room. Alvin Richardson, a 20-year plant veteran, said he remembers Cal/OSHA coming to inspect the site in 2008 and affixing an air monitor to his clothing to measure the amount of lead that he and other workers were being exposed to. Richardson says he wasn’t told the results, even though he had become a canary in the coal mine.
Experts we spoke to, including Kramer, say the results from Richardson’s air monitor, which measured airborne lead more than 13 times above levels federal limits, could have required the evacuation of workers and at a minimum should have resulted in stiff penalties.
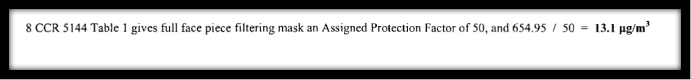
But when the results came back, Cal/OSHA may have employed some creative math. (See equation below.) Because Richardson was wearing a respirator mask, Cal/OSHA’s report reasoned its inspectors could divide the level of exposure by a factor of 50. (See formula below.) After the airborne lead levels were divided by 50, the inspection gave the smelting operation a clean bill of health, no fines were issued for the airborne lead, and the company was allowed to keep up its operation without making any engineering changes.
Cal/OSHA declined repeated requests for in-person interviews about its lead-related protocols or to comment on former workers who claim to be suffering today. In response to queries about the seemingly inadequate 2008 inspection, Cal/OSHA spokeswoman Erika Monterroza responded via email, “The division can only issue citations when it finds sufficient evidence of violations. The inspection was handled appropriately.”
But Clyde Payne, who for 23 years was the area director of U.S. OSHA’s Jackson, Mississippi, office, said that applying the equation employed by Cal/OSHA violated a fundamental OSHA principle. “The principle,” Payne said, “is you are not allowed to use the respirator to excuse toxic air. You have to implement other controls like ventilation and proper hygiene.”
Payne explained that the equation which Cal/OSHA employed is intended to be used to determine if employers are using proper respirators, or if they need to provide a better respirator. “Because we assume that workers are going to get exposed in other ways, you don’t utilize that type of division to excuse violations of the air standards.” Payne added, “There is no question it’s challenging for companies to get those levels of airborne lead down, but if you do not have somebody riding your rear end, you won’t try.”
Mariano Kramer retired in 2011 and today works as an instructor at the Dominguez Hills OSHA Training Center. After reviewing the report of the 2008 inspection of the plant, he said the levels of airborne lead that Alvin Richardson and other workers were exposed to were completely unacceptable. “One of the basic tenets of safety and health is the hierarchy of controls,” Kramer said. “You start with administrative and engineering, and the last thing that you do is personal protective equipment. Because with ventilators, you are doing nothing to correct the hazard. All you’re doing is putting a barrier to the hazard.”
First Amendment Project Lawyer: The Public Health Department “ends up being a shield for companies which expose the public and workers to toxins.”
A review of federal OSHA inspections carried out around the same time as Cal/OSHA’s 2008 inspection of Exide in Vernon does show that dramatically different standards were employed. For example, during their 2012 inspection of a Johnson Controls battery recycling plant in Ohio, OSHA inspectors affixed air monitors to workers just as they did with Richardson in California. The level of lead detected was one-third what Richardson and other Exide workers were exposed to. But because the OSHA inspectors did not employ the division formula utilized in California, they deemed the exposure levels as a “serious” violation of OSHA regulations. All told, OSHA issued to Johnson Controls Battery Group Inc. fines of $188,000, more than 1,200 times the $150 fine issued to Exide during Cal/OSHA’s 2008 inspection for violating lead standards.
Alvin Richardson told us that when he left the company in 2011 he suffered from what he believed to be lead-related symptoms, including exhaustion and tremors. After he departed his daily routine at Exide, Richardson hoped his symptoms would improve, but they worsened. Today the 53-year-old suffers from chronic weakness and kidney problems. “He can’t stand for very long,” Alvin’s wife LaShawn Richardson told us, adding that her husband had just received state disability status after a seven-year struggle.

Photo: Joanne Kim
Kramer believes that two long-running problems at Cal/OSHA likely contributed to an inadequate inspection in 2008. “The agency is kind of a political football, a battleground between those who see the prime directive as protecting workers and others who are fearful of hurting the bottom line of industry. Some staff also have a poor understanding of health-related safety issues like lead. The agency is better at recognizing a crane that might fall. When it comes to nearly invisible toxins like lead dust, that can be a problem.”
Rania Sabty-Daily, an expert in industrial hygiene and an assistant professor at California State University, Northridge, told Capital & Main that one of the stumbling blocks preventing better protection of California workers is long-delayed changes to the state’s lead standards. The standards formulated in the 1970s allow employees to continue working even with blood lead levels up to 50 μg/dL. Health experts consider those standards out of date because the U.S. Centers for Disease Control and other authorities say permanent damage can occur at levels as low as 10 μg/dL. In 2009 CDPH issued new recommendations and asked Cal/OSHA to call for removing workers with lead levels above 20 μg/dL and not returning them until they fall to below 15 μg/dL. In addition CDPH proposed that a more protective standard be applied to airborne lead.
Because CDPH can only make recommendations, CDPH petitioned Cal/OSHA in 2010 to adopt the new standards. In a statement, Cal/OSHA told us it agreed with the necessity to make some changes. “The existing lead standard is based on pre-1978 data and subsequent research has shown significant adverse effects at lower levels. The advisory committee met six times from 2011-2015 to draft a proposed industrial regulation that will lower the blood-lead removal level (BLL) and Permissible Exposure Limit (PEL). That process is ongoing.”
But the process to change California regulations appears to have bogged down. Cal/OSHA invited companies like Exide and other stakeholders to participate in advisory meetings over the new standards. During one advisory meeting in 2011, industry representatives, particularly from battery recycling companies, hammered the proposal. According to minutes from the sessions, Terry Campbell, an executive from U.S. Battery, said that one-fourth of the company’s Corona workers would have to be pulled from their jobs because of high blood-lead levels. Ultimately, the company said, it could be forced to close up shop and move to Mexico. Representatives from Exide echoed similar sentiments.
“It’s a totally dysfunctional system,” said Sabty-Daily. “We debate the toughest standards in the country — meanwhile, Cal/OSHA enforces what are among the weakest standards in the nation.”
There appears to be an even larger problem to fix. Our investigation found that workers protected by Cal/OSHA under the outdated standards continue to be harmed by unsafe lead conditions with little or no consequences.
In October we made a public records request asking CDPH for lists of workers who had lead levels at or above 20 μg/dL for the last 30 years. According to the data we received, the agency was aware of more than 26,000 blood tests from workers from more than 260 companies across the state. Workers were counted once per year at their highest level according to CDPH. We also learned that between 2010 and 2017, even as California’s regulatory agencies continued to debate toughening lead standards, CDPH was aware of an additional 2,256 blood tests at or above 20 μg/dL. Despite those alarming numbers, finding the locations of the workplaces that have had large numbers of lead poisoned workers is for the moment impossible.
Although CDPH previously provided year-by-year anonymous data for lead-poisoned workers at Exide, the agency turned down our request for information about where those other cases in the state were occurring. Citing a “constitutional right to privacy,” CDPH says it is concerned that providing anonymous details about the extent of the problem at specific companies could somehow lead to identifying the individual workers. When there is “a high risk of re-identification, statistical masking must be applied,” the agency said in a March 14 statement.
Dr. Bruce Lanphear, the lead-poisoning expert, also was troubled by the withholding of specific numbers for where the lead poisoning incidents were occurring. “That’s just hogwash. One of the basic functions of public health is to make clear the extent of the problem and where it’s occurring. You can’t protect the public if you’re not armed with the information.”
James Wheaton, senior counsel for the First Amendment Project and a media-law professor at the University of California, Berkeley, called the agency’s rationale for keeping the information secret “bogus” and said he believed the agency had violated California law with its refusal to disclose the information.
“CDPH unfortunately has a tendency to jealously guard information which is vital to the public,” Wheaton said. “The net result is the agency ends up being a shield for companies which expose the public and workers to toxins.”
While Exide closed in 2015, several battery recycling plants continue to operate in the greater Los Angeles area, and they appear to represent an ongoing problem when it comes to workers exposed to lead. While CDPH would not provide Capital & Main with information about where the most serious cases are occurring, in response to a public records request the agency did provide similar data to the Los Angeles Times in 2016 for worker exposures in Los Angeles County from 2008 to 2014.
The data, provided to Times reporter Tony Barboza, show that Quemetco, another Los Angeles-area recycling plant which, unlike Exide, is still up and running, had 254 workers with elevated blood-lead levels (at or above 10 g/dL) between 2008 and 2014. By comparison, Exide had 175 workers during that same time period with similarly elevated levels. Quemetco also appears to have another Exide-like problem. Soil samples taken from homes within a quarter-mile of the plant, according to data we obtained from the Department of Toxic Substances Control, also show that surface soil is on average four times above acceptable levels, suggesting a multimillion-dollar cleanup could be necessary.
Prior to publication of this article we shared data we had gathered with several lawmakers and Bill Allayaud, the California director of the Environmental Working Group, a science-based watchdog organization. Allayaud’s group has spearheaded several proposed lead laws in California. “We all know how the neighborhoods around Exide were polluted with toxic lead over the long term, and now we are finding out how workers on the frontlines were neglected by the agencies that are supposed to monitor and demand that hazardous conditions be eliminated,” Allayaud said. “This needs to be fixed so this never happens again.”
Allayaud collaborated with San Jose Assemblyman Ash Kalra, who introduced legislation sponsored by the Environmental Working Group that would require CDPH and Cal/OSHA to follow federal standards recognized in other states. Kalra’s measure, Assembly Bill 2963, would legally require the “State Department of Public Health to report to the Division of Occupational Safety and Health any instance where a worker’s blood-lead level is at or above a certain amount.”
In a statement to Capital & Main, Kalra said, “Lead poisoning is a serious matter and we need to consider the gravity of this hazard by ensuring that our state agencies are properly scrutinizing cases involving workers’ exposure to high levels of lead — this means that adequate inspections need to be carried out whenever there is evidence of serious lead-related exposure.”
Kalra plans to hold hearings in April for his worker-protection bill based on our investigations. He told Capital & Main that he would like to have Alvin Richardson and other workers testify to educate the public about what it’s like to experience lead poisoning.
“Alvin’s a proud man,” said Richardson’s wife, LaShawn. “Going through this has been a long, incredibly difficult struggle for our entire family.” She said she was speaking to us in the hope that future workers wouldn’t have to endure what her husband has.
Joe Rubin wrote this story while participating in the California Data Fellowship, a program of USC’s Center for Health Journalism.
Tomorrow —
California Has Worse Lead Standards Than Arkansas and Texas. Why?
Copyright Capital & Main

-

 The SlickJanuary 27, 2026
The SlickJanuary 27, 2026The One Big Beautiful Prediction: The Energy Transition Is Still Alive
-

 Column - State of InequalityJanuary 29, 2026
Column - State of InequalityJanuary 29, 2026Are California’s Billionaires Crying Wolf?
-

 Latest NewsFebruary 3, 2026
Latest NewsFebruary 3, 2026Amid the Violent Minnesota Raids, ICE Arrests Over 100 Refugees, Ships Many to Texas
-

 Dirty MoneyJanuary 30, 2026
Dirty MoneyJanuary 30, 2026Amid Climate Crisis, Insurers’ Increased Use of AI Raises Concern For Policyholders
-

 Featured VideoFebruary 4, 2026
Featured VideoFebruary 4, 2026Protesters Turn to Economic Disruption to Fight ICE
-

 The SlickFebruary 2, 2026
The SlickFebruary 2, 2026Colorado May Ask Big Oil to Leave Millions of Dollars in the Ground
-

 Column - State of InequalityFebruary 5, 2026
Column - State of InequalityFebruary 5, 2026Lawsuits Push Back on Trump’s Attack on Child Care
-

 Column - California UncoveredFebruary 6, 2026
Column - California UncoveredFebruary 6, 2026What It’s Like On the Front Line as Health Care Cuts Start to Hit


